Implant rehabilitation of extremely atrophic mandibles (Cawood and Howell Class VI) with a fixed-removable solution supported by four implants: one-year results from a preliminary prospective case series study
June 14, 2017 / Categories: Digital Dentistry, Implant Dentistry

Tallarico, Marco

Xhanari, Erta

Kadiu, Blerina

Scrascia, Roberto
Abstract
Objective
The objective of this study was to report one-year preliminary data on Cawood and Howell Class VI patients rehabilitated with a fixed-removable solution.
Materials and methods
Completely edentulous patients, aged 18 years or older, presenting with severely atrophic mandibles (Class VI according to Cawood and Howell) were enrolled and treated using four implants, a CAD/CAM titanium bar and a low-profile attachment system to support an implant-supported overdenture. Outcome measures were success rates of the implants and prosthesis, complications, marginal bone level changes, bleeding index, plaque index and patient satisfaction (Oral Health Impact Profile).
Results
A total of 16 Osstem TSIII implants were placed in four consecutive edentulous participants. All of the treated patients were female with an average age of 71.5 (range: 64–82). Patients were followed up for a mean period of 13.8 months (range: 12–16) after loading. No participants dropped out, and no deviation from the original protocol occurred. At the one-year follow-up, no implants or prosthesis had failed and no biological or technical complications had occurred. At the one-year follow-up, the mean marginal bone loss was 0.23 ± 0.07 mm. The Oral Health Impact Profile summary scores demonstrated a significant decrease throughout the study, from 66.5 ± 3.7 to 19.3 ± 2.8. At the one-year follow-up, the bleeding index was 1.6% and the plaque index was 4.7%.
Conclusion
Within the limitations of this study, an overdenture fully supported by four implants and a CAD/CAM titanium bar with a low-profile attachment system, can be considered an effective and predictable option for patients with Cawood and Howell Class VI atrophic mandibles. Minimum marginal bone remodeling, good periodontal parameters and patient satisfaction can be expected.
Keywords
Implant, atrophic mandible, CAD/CAM titanium bar, overdenture.
Introduction
Prosthetic rehabilitation on implants in severely atrophic patients is a challenge. In a Cawood and Howell Class VI case, the mandible presents with a depressed ridge form, inadequate in height and width, evident basilar bone loss, and alveolar nerve exposure.1Cawood JI, Howell RA. A classification of the edentulous jaws.
→ Int J Oral Maxillofac Surg. 1988 Aug;17(4):232–6.
A mandibular implant overdenture is a viable treatment option for edentulous mandibles, improving overall patient satisfaction compared with a removable complete denture.2Muller F, Duvernay E, Loup A, Vazquez L, Herrmann FR, Schimmel M. Implantsupported mandibular overdentures in very old adults: a randomized controlled trial.
→ J Dent Res. 2013 Dec;92(12 Suppl):154S–60S. These studies document successful treatment outcomes and better oral health-related quality of life as compared with wearing of complete dentures.3Harris D, Höfer S, O’Boyle CA, Sheridan S, Marley J, Benington IC, Clifford T, Houston F, O’Connell B. A comparison of implant-retained mandibular overdentures and conventional dentures on quality of life in edentulous patients: a randomized, prospective, within-subject controlled clinical trial.
→ Clin Oral Implants Res. 2013 Jan;24(1):96–103. The number of implants to be placed and the type of retention have been controversially discussed.4Andreiotelli M, Att W, Strub JR. Prosthodontic complications with implant overdentures: a systematic literature review.
→ Int J Prosthodont. 2010 May-Jun;23(3):195–203.5Alsabeeha NH, Payne AG, Swain MV. Attachment systems for mandibular two-implant overdentures: a review of in vitro investigations on retention and wear features.
→ Int J Prosthodont. 2009 Sep-Oct;22(5):429–40.6Roccuzzo M, Bonino F, Gaudioso L, Zwahlen M, Meijer HJ. What is the optimal number of implants for removable reconstructions? A systematic review on implant-supported overdentures.
→ Clin Oral Implants Res. 2012 Oct;23 Suppl 6:229–37. The implant survival rate of mandibular overdentures is high regardless of the number of implants.7Lee JY, Kim HY, Shin SW, Bryant SR. Number of implants for mandibular implant overdentures: a systematic review.
→ J Adv Prosthodont. 2012 Apr;4:204–9. Therefore, two single standing implants with ball attachments have sometimes been considered a risk and some investigators suggest using four implants with a splinting bar.8Roccuzzo M, Bonino F, Gaudioso L, Zwahlen M, Meijer HJ. What is the optimal number of implants for removable reconstructions? A systematic review on implant-supported overdentures.
→ Clin Oral Implants Res. 2012 Oct;23 Suppl 6:229–37.9Naert I, Gizani S, Vuylsteke M, van Steenberghe D. A randomised clinical trial on the influence of splinted and unsplinted oral implants in mandibular overdenture therapy. A 3-year report.
→ Clin Oral Investig. 1997 Jun;1(2):81–8.10Batenburg RH, Raghoebar GM, Van Oort RP, Heijdenrijk K, Boering G. Mandibular overdentures supported by two or four endosteal implants. A prospective, comparative study.
→ Int J Oral Maxillofac Surg. 1998 Dec;27(6):435–9.11Weinländer M, Piehslinger E, Krennmair G. Removable implant-prosthodontic rehabilitation of the edentulous mandible: five-year results of different prosthetic anchorage concepts.
→ Int J Oral Maxillofac Implants. 2010 May-Jun;25(3):589–97.
In patients with an alternated skeletal maxillomandibular relationship, a fixed-removable solution may be a viable option for soft- and hard-tissue reconstruction and for the All-on-4 concept for the rehabilitation of patients presenting with extremely atrophic mandibles (Cawood and Howell Class VI).12Cawood JI, Howell RA. A classification of the edentulous jaws.
→ Int J Oral Maxillofac Surg. 1988 Aug;17(4):232–6.13Pozzi A, Tallarico M, Moy PK. Four-implant overdenture fully supported by a CAD-CAM titanium bar: a single-cohort prospective 1-year preliminary study.
→ J Prosthet Dent. 2016 Oct;116(4):516–23.
A fixedremovable solution may be a feasible option to overcome the technical complications of other treatment options.14Andreiotelli M, Att W, Strub JR. Prosthodontic complications with implant overdentures: a systematic literature review.
→ Int J Prosthodont. 2010 May-Jun;23(3):195–203.15Tallarico M, Meloni MS, Xhanari E, Canullo L. Three-year clinical and radiographic outcomes of patients treated according to the All-on-4 concept in the daily practice: a prospective observational study on implants and prosthesis survival rates and complications.
→ J Oral Science Rehabilitation. 2016 Jun;2(2):16–25. Moreover, hygienic maintenance of the prosthesis can be challenging when extensive prosthetic flanges are needed to provide adequate lip and check support to overcome esthetic problems typical of aging.16Abi Nader S, Eimar H, Momani M, Shang K, Daniel NG, Tamimi F. Plaque accumulation beneath maxillary All-on-4 implantsupported prostheses.
→ Clin Implant Dent Relat Res. 2015 Oct;17(5):932–7.
The purpose of this preliminary case series study was to report one-year preliminary data on Cawood and Howell Class VI patients rehabilitated with a fixed-removable solution. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology reporting guidelines.17Elm von E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. STROBE Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies.
→ J Clin Epidemiol. 2008 Apr;61(4):344–9.
Materials and methods
This preliminary investigation was designed as a prospective study conducted according to the principles embodied in the Helsinki Declaration of 1975, as revised in 2008. Completely edentulous patients, aged 18 years or older, presenting with severely atrophic mandibles (Class VI according to Cawood and Howell)1 were enrolled and treated in consecutive order after being informed about the nature of the study and providing their written informed consent. All of the surgical and prosthetic procedures were performed in a private center in Rome, Italy, by a certified implantologist (MT) between September 2015 and February 2016. Exclusion criteria were general contraindications to oral surgery, pregnancy or nursing, intravenous bisphosphonate therapy, alcohol or drug abuse, heavy smoking (≥ 10 cigarettes/day), radiation therapy to the head or neck region within the last five years, parafunctional activity, untreated periodontitis, full-mouth bleeding on probing, and a full-mouth plaque index of ≤ 25%, and allergy or adverse reactions to the restorative materials.
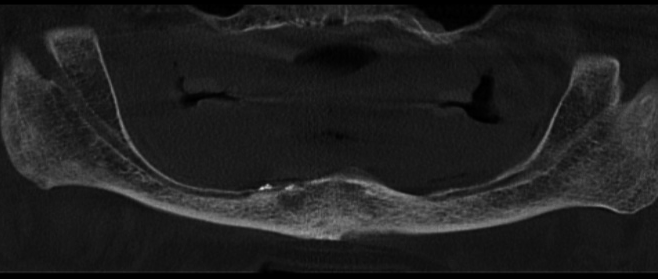
Preoperative photographs, radiographs (Figs. 1a–c) and model casts were produced for initial screening and case evaluation. A radiographic guide was made by duplicating the relined pre-existent removable complete mandibular denture, if judged viable from an esthetic and functional perspective; otherwise, a new radiographic guide was made according to the functional and esthetic requirements. A cone beam computed tomography (CBCT) scan (CRANEX 3Dx, SOREDEX, Tuusula, Finland) was taken of each enrolled patient wearing the radiographic guide and a bite index in centric occlusion with an extraoral volume transfer element (Evobite, 3DIEMME, Cantù, Italy), fixed using a dedicated silicone material (3DIEMME). Then, the radiographic guide and the bite index were repositioned in the master cast and optical scanning was performed. Radiographic and prosthetic data were imported into a dedicated diagnostic and medical imaging software (3Diag nosys 4.2, 3DIEMME). The digitalized model and radiographic guide were accurately superimposed over the reconstructed bone volume by CBCT, based on the volumetric elements, present in both the CBCT volume and the optical scan (Evobite). Four implants per patient were planned in the anterior area of the mandible, according to the prosthetic setup. After careful functional and esthetic evaluation and final verification, the prosthetic- driven plan was approved, and a stereolithographic surgical template was fabricated with a newer rapid prototyping technology (New Ancorvis, Bargellino, Italy).
- Fig. 1a
- Fig. 1c
- Fig. 1b
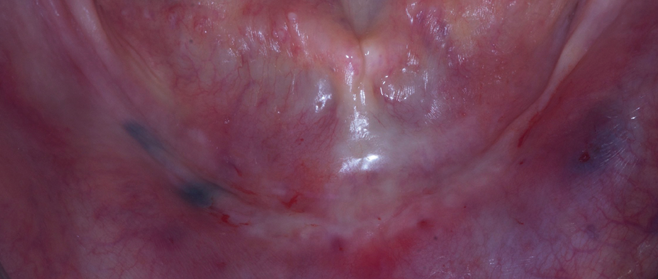
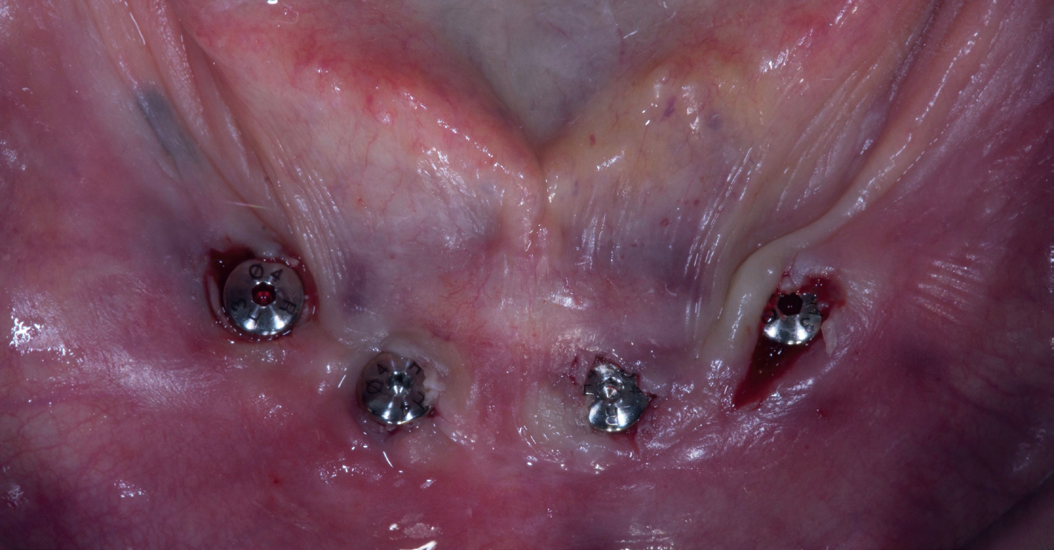
One hour before implant placement, patients received a single dose of an antibiotic (2 g of amoxicillin or 600 mg of clindamycin if allergic to penicillin) and professional hygiene therapy. Prior to the start of surgery, the patients rinsed with 0.2% chlorhexidine for 1 min. The surgical template (New Ancorvis) was fitted in the patient’s mouth, then local anesthesia was administered with a 4% articaine solution with 1:100,000 epinephrine (Ubistein, 3M ESPE, Milan, Italy). The implants were placed in the planned anatomical sites according to a onestage approach (Figs. 2a & b)18Tallarico M, Vaccarella A, Marzi GC. Clinical and radiological outcomes of 1- versus 2-stage implant placement: 1-year results of a randomised clinical trial.
→ Eur J Oral Implantol. 2011 Spring;4(1):13–20. using the surgical template. Each patient received four Osstem TSIII bone level implants (Osstem TSIII, Osstem, Seoul, South Korea), placed either without a flap or with a minimally invasive flap, according to the drilling protocol recommended by the manufacturer (OsstemGuide Kit). After surgery, the existing removable complete denture was relined chairside (Sofreliner Tough Soft, Tokuyama Dental, Montecchio Precalcino, Vicenza, Italy) to accommodate the healing of the hard and soft tissue, thereby ensuring no pressure on the healing abutments. Occlusion was checked during osseointegration of the implants.
- Fig. 2a
- Fig. 2b
After implant placement, all of the patients received oral and written recommendations on medication, oral hygiene maintenance and diet. Analgesics (500 mg of paracetamol plus 30 mg of codeine, or 600 mg of ibuprofen) were administered as needed. Eight weeks later, a definitive impression was taken using plaster (Snow White Plaster No. 2, Kerr, Orange, Calif. U.S.) as both splinting and impression material (Fig. 3).19Pozzi A, Tallarico M, Mangani F, Barlattani A. Different implant impression techniques for edentulous patients treated with CAD/ CAM complete-arch prostheses: a randomised controlled trial reporting data at 3 year postloading.
→ Eur J Oral Implantol. 2013 Winter;6(4):325–40. A complete mounting technique was used to articulate the opposite arch cast (KaVo PROTARevo 7, KaVo Dental, Biberach, Germany). Then, esthetics and function of the final occlusal vertical dimension, tooth position and interocclusal record were verified and approved by both the clinician and the patient at the try-in appointment. Afterward, the master cast and the try-in were digitalized with an optical scanner (Identica T500, Medit, Seoul, South Korea).
- Fig. 3
Figs. 1a-c
Preoperative radiographs (a & b) and intraoral photograph (c).
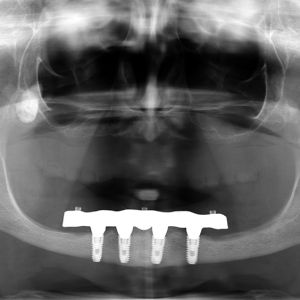
Figs. 2a-b
IClinical view (a) after placement of the four implants (Osstem TSIII, 4.5 × 10 mm) according to a one-stage protocol. Radiograph after implant placement (b).
Fig. 3
Definitive impression taken using plaster as both splinting and impression material.
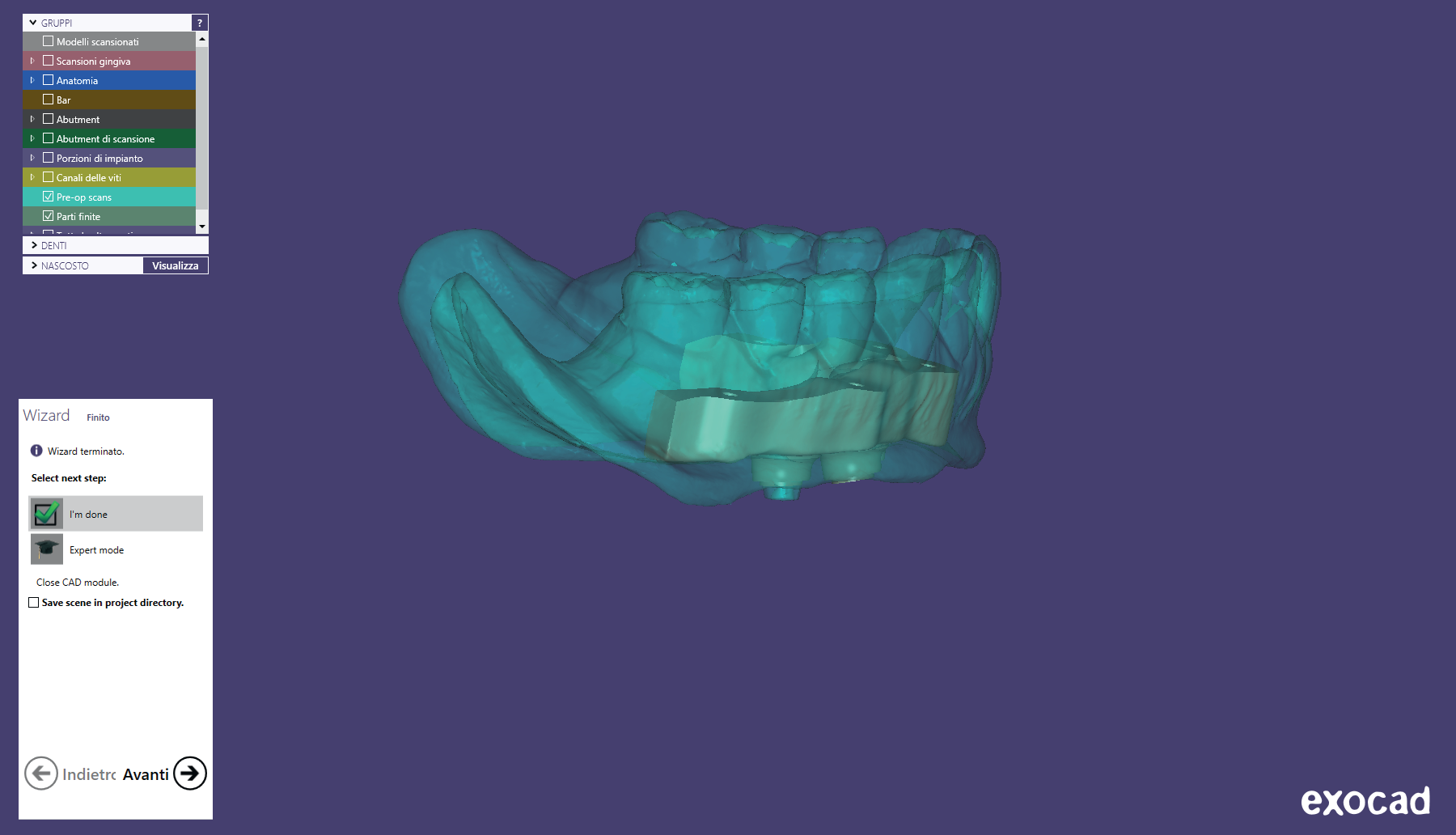
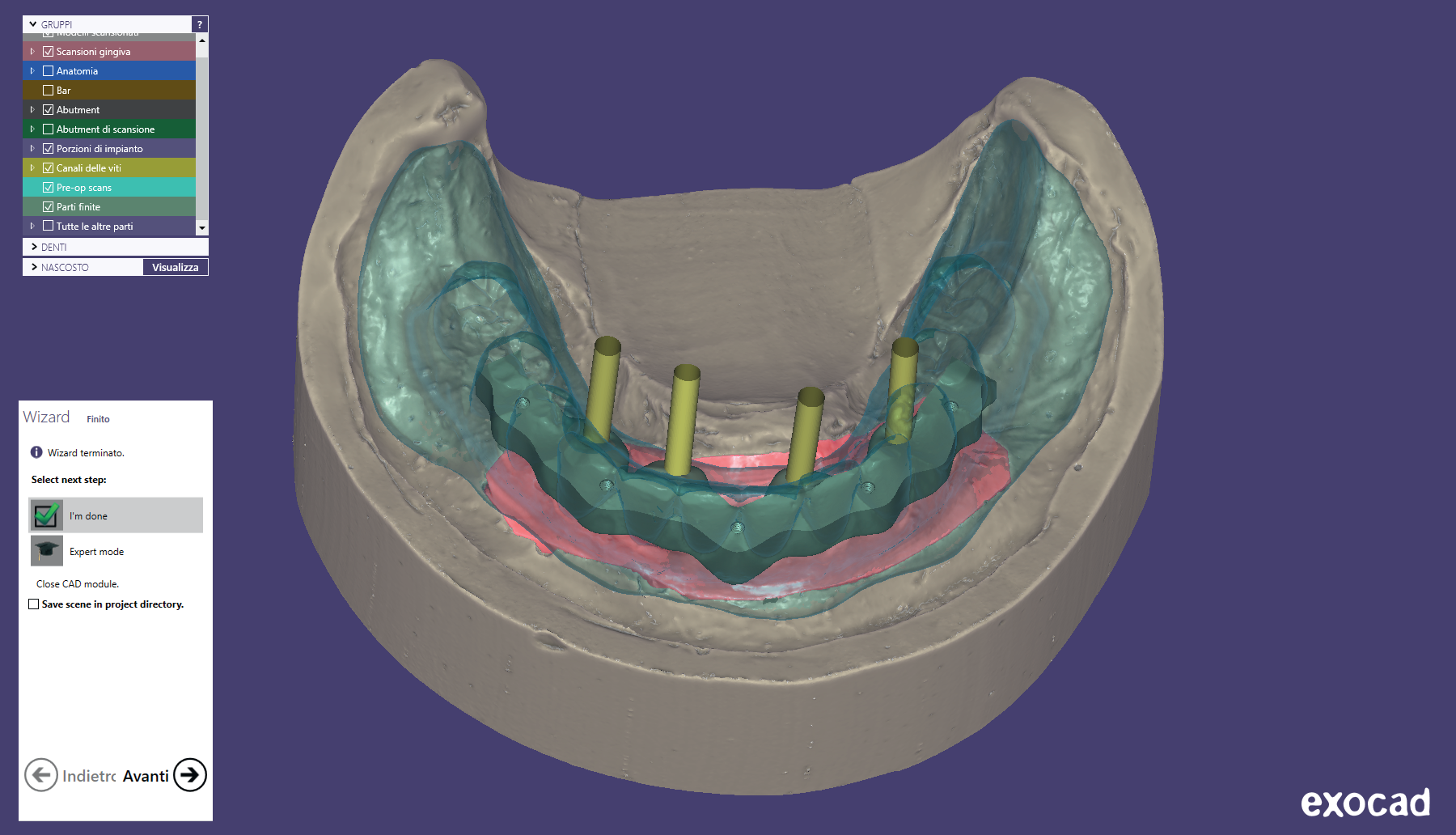
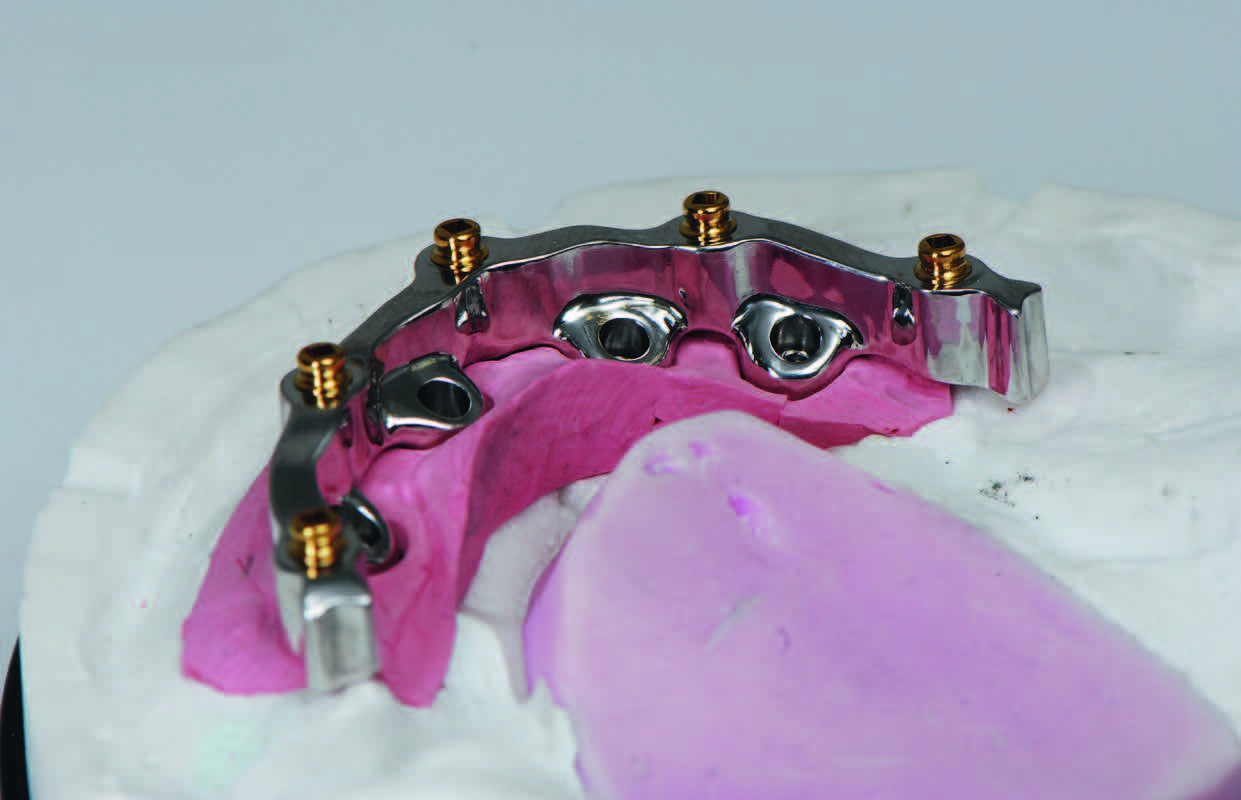
A CAD/CAM titanium bar was virtually designed (Figs. 4a & b) according to the ridge and prosthetic contours and implant position in order to enhance a vertical path of insertion of between 4 and 6°. Then, a one-piece titanium bar was manufactured (Fig. 5) from a homogenous solid block of a medical titanium alloy (Ti6Al4V, New Ancorvis). Four to five threadable OT Equator attachments (Rhein 83, Bologna, Italy) were placed along the implant bar.
The fit of the implant bar was clinically and radiographically tested in the patient’s mouth according to a previously published protocol.20Abduo J, Bennani V, Waddell N, Lyons K, Swain M. Assessing the fit of implant fixed prostheses: a critical review.
→ Int J Oral Maxillofac Implants. 2010 May-Jun;25(3):506–15.21Eisenmann E, Mokabberi A, Walter MH, Freesmeyer WB. Improving the fit of implant-supported superstructures using the spark erosion technique.
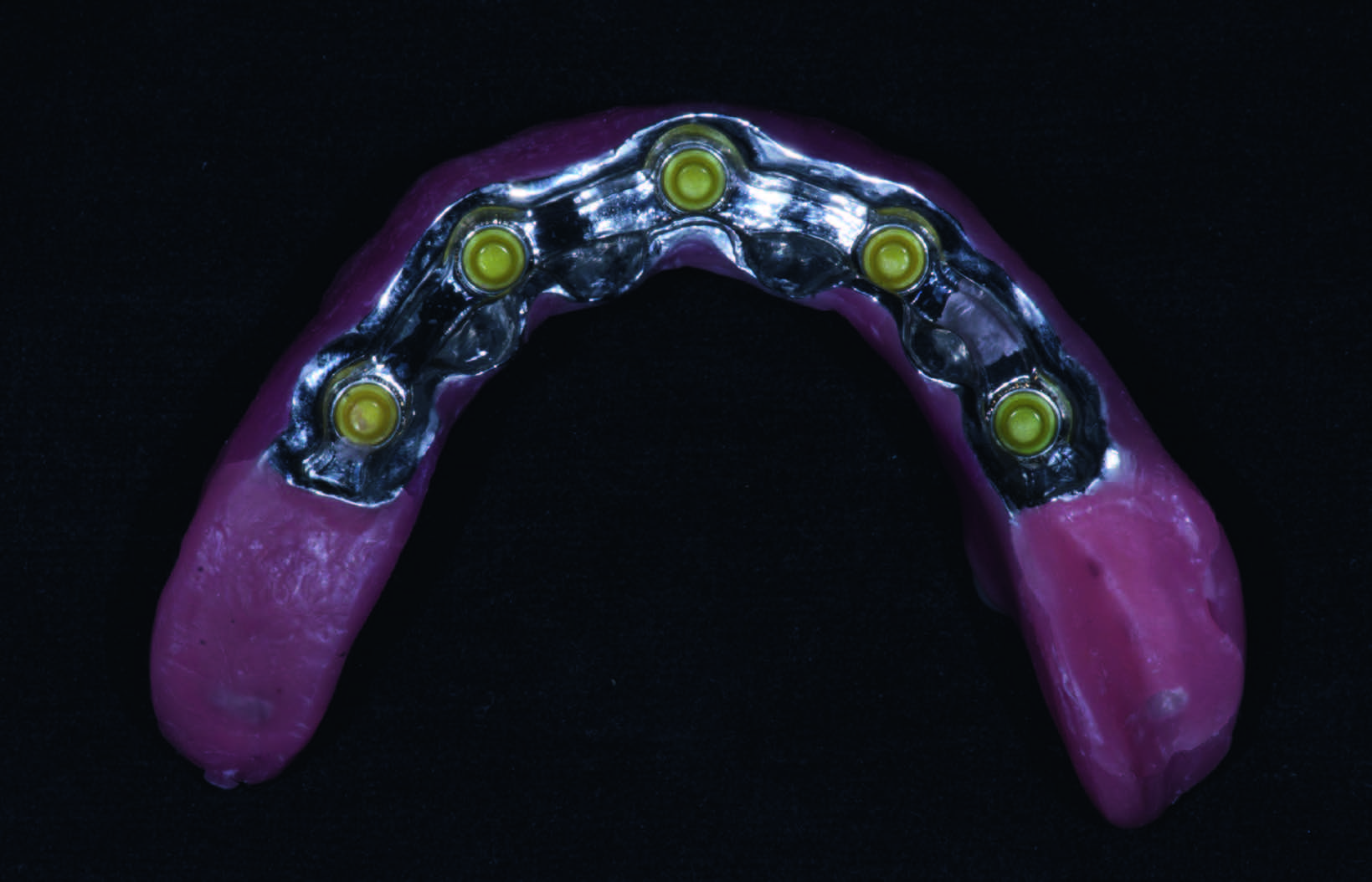
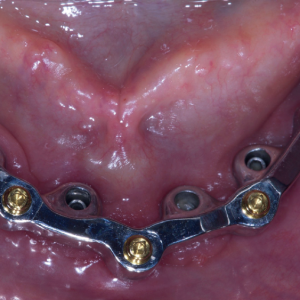
→ Int J Oral Maxillofac Implants. 2004 Nov-Dec;19(6):810–8. A cast cobalt–chromium alloy metal framework (Vitallium, DENTSPLY International, York, Pa., U.S.) was conventionally fabricated on to the CAD/ CAM titanium bar as a counterpart (Fig. 6). Finally, the overdenture was finished, sealing the borders to minimize food impaction and saliva and air leakage. The titanium bar was screwed at the abutment level according to the manufacturer’s instructions, and the fixed-removable solution was delivered (Figs. 7a–c). All of the patients were then enrolled in a standard implant recall program.
Oral hygiene maintenance was checked and radiographs were taken early after final prosthesis delivery. Occlusion was checked at every appointment (Figs. 8a & b).
- Fig. 4a
- Fig. 4b
- Fig. 5
- Fig. 6
- Fig. 7a
- Fig. 7b
- Fig. 7c
- Fig. 8a
- Fig. 8b
Figs. 4a-b
CAD/CAM images showing the titanium bar project, according to the prosthetic volume of the overdenture (a) and the relationship between the titanium bar and implants placed (b).
Fig. 5
CAD/CAM titanium bar.
Fig. 6
Metallic counterpart of the overdenture.
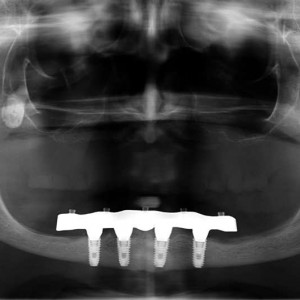
Figs. 7a-c
Clinical view of the overdenture at the time of prosthesis delivery (a & b) and radiographic view early after final prosthesis delivery (c).
Figs. 8a-b
One-year follow-up of a mandibular CAD/CAM titanium bar screwed on to implants (a). Dental panoramic tomogram taken one year after loading, showing the perfect fit of the bar on the implants (b).
Outcome measures
The primary outcome measures were the following:
- Success rates of the implants and prosthesis: An implant was considered a failure if it presented with any mobility, assessed by tapping or rocking the implant head with the metallic handles of two instruments, progressive marginal bone loss or infection, and any mechanical complications rendering the implant unusable, although still mechanically stable in the bone. A prosthesis was considered a failure if it needed to be replaced with another prosthesis.
- Complications: Any biological (pain, swelling, suppuration, etc.) and/or mechanical (screw loosening, fracture of the framework and/or the veneering material, etc.) complications were evaluated.
- Marginal bone levels: The levels were assessed using intraoral digital periapical radiographs (Digora Optime, SOREDEX; photostimulable phosphor imaging plate, size 2, pixel size of 30 μm, resolution of 17 lp/mm) at implant placement (baseline) and one year after loading. Intraoral radiographs were taken with the paralleling technique by means of a periapical radiograph with a commercially available film holder (Rinn XCP, Dentsply Rinn, Elgin, Ill., U.S.). The radiographs were accepted or rejected for evaluation based on the clarity of the implant threads. All readable radiographs were uploaded to an image analysis software package (DfW 2.8, SOREDEX) that was calibrated using the known length or diameter of the dental implants and displayed on a 24 in. LCD screen (iMac, Apple, Calif., U.S.) and evaluated under standardized conditions (ISO 12646:2004). The marginal bone levels were determined from linear measurements performed by an independent calibrated examiner on each periapical radiograph, from the mesial and distal margin of the implant neck to the most coronal point where the bone appeared to be in contact with the implant. – Patient satisfaction with function and esthetics was assessed using a scale of 1–10, where 10 = fully satisfied, 5 = satisfied and 1 = not satisfied. Quality of life was assessed by the Oral Health Impact Profile (OHIP-21) questionnaire, which was completed by the participants. The questionnaire consists of seven subscales (functional limitations, physical pain, psychological discomfort, physical disability, psychological disability, social disability, and handicap) with two to four questions each. Participants chose from five possible responses for each question as follows: never, hardly ever, occasionally, fairly often and very often. Items were scored on a five-point ordinal scale ranging from 1 (never) to 5 (very often). Lower OHIP total scores are suggestive of improvement in oral health-related quality of life.
The questionnaire was administered before treatment and one year after definitive prosthesis delivery. - Bleeding index and plaque index were evaluated at four sites around each implant– abutment interface at the one-year examination with a periodontal probe (PCPUNC156, Hu-Friedy, Milan, Italy).
An independent dentist (EX) evaluated the implant and prosthetic survival and success rates and administered the patient satisfaction and OHIP questionnaires. Complications were assessed and treated by the treating clinician (MT), who was nonblinded. Marginal bone level changes were evaluated by an independent radiologist. An independent blinded dental hygienist who was otherwise not involved in the study performed all of the periodontal measurements.
All data analysis was carried out according to a pre-established analysis plan using software (IBM SPSS Statistics for Macintosh, Version 22.0, IBM, Armonk, N.Y., U.S.). Descriptive analy sis was performed using means, standard deviations and a 95% confidence interval. Comparison of the means for marginal bone level changes, patient satisfaction and OHIP scores between the baseline and one-year follow-up examinations was performed by paired tests.
A biostatistician with expertise in dentistry analyzed the data.
Results
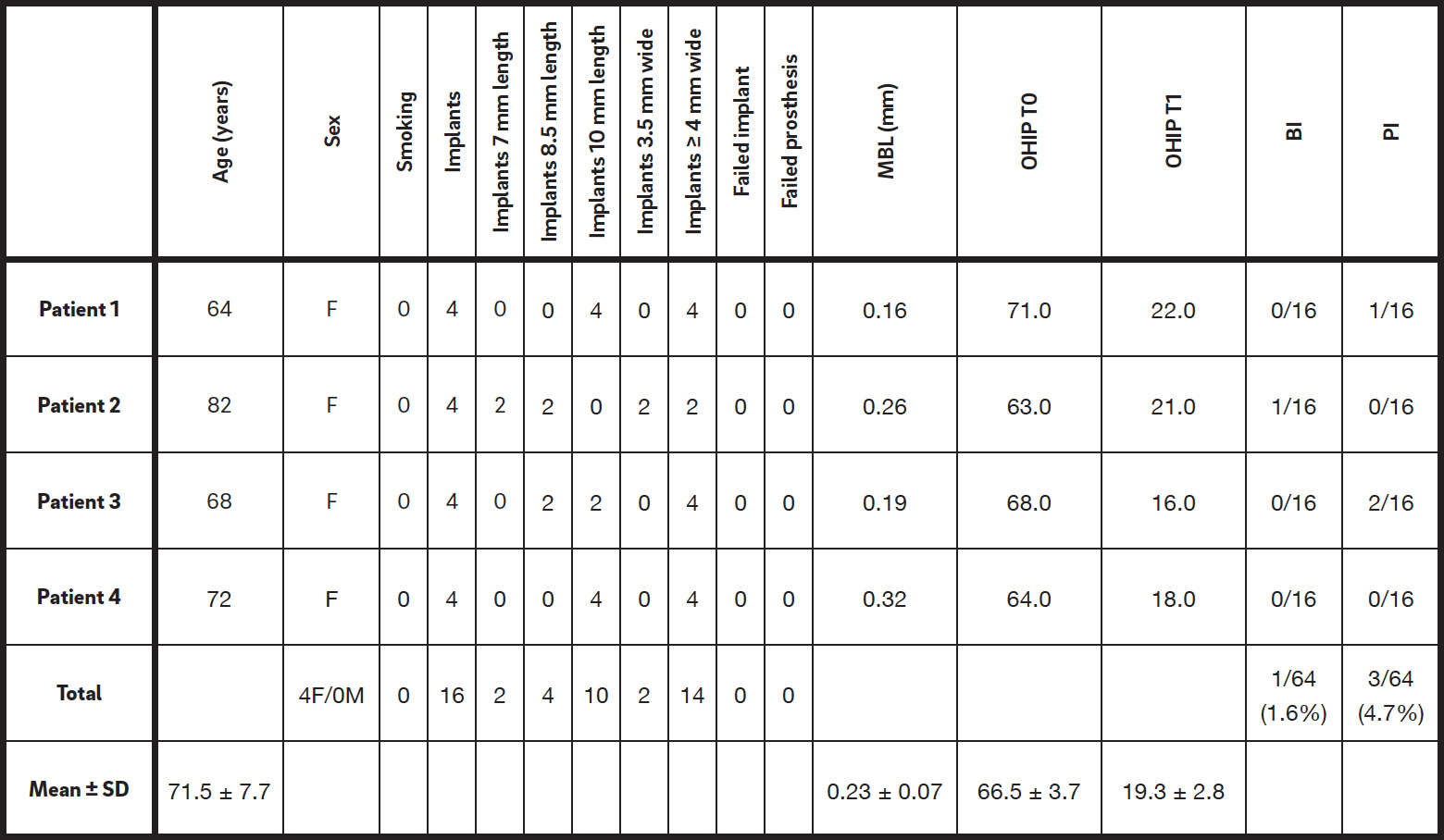
A total of 16 Osstem TSIII implants (14 regular platform and two mini platform) were placed in four consecutive edentulous participants. All of the participants were followed up for a minimum of one year (mean: 13.8 months; range: 12–16) after definitive loading. All of the treated patients were female with an average age of 71.5 (range: 64–82). The main patient and implant characteristics are shown in Table 1. No participants dropped out, and no deviation from the original protocol occurred. At the one-year follow- up, no implants or prosthesis had failed, resulting in cumulative implant and prosthetic survival rates of 100%. No biological or technical complications occurred during the followup, resulting in cumulative implant and prosthetic success rates of 100%. At the one-year follow- up, the mean marginal bone loss was 0.23 ± 0.07 mm. The OHIP summary scores demonstrated a significant decrease (P = 0.0002) throughout the study, from 66.5 ± 3.7 to 19.3 ± 2.8. At the one-year followup, the bleeding index was 1.6% and the plaque index was 4.7%. All of the data are summarized in Table 1.
Table 1
Characteristics and results of included patients/implants.
Discussion
This prospective study was designed to evaluate the one-year clinical and radiographic outcomes and patient satisfaction of Cawood and Howell Class VI patients treated with a fixedremovable overdenture supported by four implants, placed using guided surgery, and a CAD/ CAM titanium bar. Because it was designed as a single-cohort, proof-of-concept study, the main limitations were the lack of a control group and a small sample size. Hence, this investigation should be considered as a pilot for future multicenter randomized clinical trials with control group comparison.
The results of the present one-year preliminary prospective case series study reported implant and prosthetic survival and success rates of 100% and greater patient satisfaction, indicating that patients with extremely atrophic mandibles (Cawood and Howell Class VI) may be rehabilitated using this fixed-removable solution.
Complete maxillary and mandibular dentures have been the conventional standard of care for edentulous patients. However, most patients report significant problems adapting to their mandibular dentures owing to a lack of comfort, retention and stability and to the inability to chew and eat properly, resulting in pain and discomfort. Recent evidence from studies carried out over the past decade has determined that the two-implant overdenture is considered the first alternative treatment for the completely edentulous mandible.22Fitzpatrick B. Standard of care for the edentulous mandible: a systematic review.
→ J Prosthet Dent. 2006 Jan;95(1):71–8.23Burns DR. Mandibular implant overdenture treatment: consensus and controversy.
→ J Prosthodont. 2000 Mar;9(1):37–46. Nevertheless, the placement of at least four implants of standard length may allow the delivery of an overdenture supported by a CAD/CAM titanium bar and a low-profile attachment system,24Zitzmann NU, Marinello CP. Treatment plan for restoring the edentulous maxilla with implant-supported restorations: removable overdenture versus fixed partial denture design.
→ J Prosthet Dent. 1999 Aug;82(2):188–96.
avoiding any bearing area on the soft tissue and reducing the denture base extension.25Jemt T, Book K, Linden B, Urde G. Failures and complications in 92 consecutively inserted overdentures supported by Brånemark implants in severely resorbed edentulous maxillae: a study from prosthetic treatment to first annual check-up.
→ Int J Oral Maxillofac Implants. 1992 Summer;7(2):162–7. The OT Equator for bars exists in two types, castable and prefabricated (threadable). In the present study, the prefabricated shape was used. This type of attachment is initially of higher cost, but it is highly wear resistant, its surface being of titanium nitride. Furthermore, it is easy to replace, if needed.
A fixed dental prosthesis on four implants may be a possible alternative to a mandibular overdenture on four implants and supported by a CAD/CAM titanium bar with a low-profile attachment system. Nevertheless, it is associated with higher marginal bone loss, high frequency of complications and poor plaque control, particularly in extremely atrophic patients.26Patzelt SB, Bahat O, Reynolds MA, Strub JR. The all-on-four treatment concept: a systematic review.
→ Clin Implant Dent Relat Res. 2014 Dec;16(6):836–55.27Sadowsky SJ. Treatment considerations for maxillary implant overdentures: a systematic review.
→ J Prosthet Dent. 2007 Jun;97(6):340–8.28Tallarico M, Canullo L, Pisano M, Peñarrocha-Oltra D, Peñarrocha-Diago M, Meloni SM. An up to 7-year retrospective analysis of biologic and technical complication with the All-on-4 concept.
→ J Oral Implantol. 2016 Jun;42(3):265–71.29Tallarico M, Canullo L, Pisano M, Peñarrocha-Oltra D, Peñarrocha-Diago M, Meloni SM. An up to 7-year retrospective analysis of biologic and technical complication with the All-on-4 concept.
→ J Oral Implantol. 2016 Jun;42(3):265–71. In the present study, a trend of minimum marginal bone loss and good periodontal parameters was observed within the one-year follow-up, demonstrating that a good level of hygiene can be expected using this fixed-removable solution. Similar to with a fixed dental prosthesis, patient satisfaction significantly improves owing to an improvement in esthetics and masticatory function. Moreover, the prosthetic flanges of a fixedremovable solution allow for full lip and cheek support.
Conclusion
Within the limitations of this study, a mandibular overdenture on four implants and supported by a CAD/CAM titanium bar with a low-profile attachment system can be considered an effective and predictable option for patients with Cawood and Howell Class VI atrophic mandibles. Minimum marginal bone remodeling, good periodontal parameters and patient satisfaction can be expected.
Competing interests
MT is the Research Project Manager at Osstem AIC, Italy. However, this study was selfsupported. Hence, the authors declare no conflicts of interest.
Why did you conduct the research reported on in this paper?
For what reasons could others cite your paper?
How could your study’s findings have an impact on dentistry?
What is the relevance of your study’s findings to the daily practice of a dentist?
What are your recommendations for further investigation of the topic of your article?
References
| 1, 12. | ↑ | Cawood JI, Howell RA. A classification of the edentulous jaws. → Int J Oral Maxillofac Surg. 1988 Aug;17(4):232–6. |
| 2. | ↑ | Muller F, Duvernay E, Loup A, Vazquez L, Herrmann FR, Schimmel M. Implantsupported mandibular overdentures in very old adults: a randomized controlled trial. → J Dent Res. 2013 Dec;92(12 Suppl):154S–60S. |
| 3. | ↑ | Harris D, Höfer S, O’Boyle CA, Sheridan S, Marley J, Benington IC, Clifford T, Houston F, O’Connell B. A comparison of implant-retained mandibular overdentures and conventional dentures on quality of life in edentulous patients: a randomized, prospective, within-subject controlled clinical trial. → Clin Oral Implants Res. 2013 Jan;24(1):96–103. |
| 4, 14. | ↑ | Andreiotelli M, Att W, Strub JR. Prosthodontic complications with implant overdentures: a systematic literature review. → Int J Prosthodont. 2010 May-Jun;23(3):195–203. |
| 5. | ↑ | Alsabeeha NH, Payne AG, Swain MV. Attachment systems for mandibular two-implant overdentures: a review of in vitro investigations on retention and wear features. → Int J Prosthodont. 2009 Sep-Oct;22(5):429–40. |
| 6, 8. | ↑ | Roccuzzo M, Bonino F, Gaudioso L, Zwahlen M, Meijer HJ. What is the optimal number of implants for removable reconstructions? A systematic review on implant-supported overdentures. → Clin Oral Implants Res. 2012 Oct;23 Suppl 6:229–37. |
| 7. | ↑ | Lee JY, Kim HY, Shin SW, Bryant SR. Number of implants for mandibular implant overdentures: a systematic review. → J Adv Prosthodont. 2012 Apr;4:204–9. |
| 9. | ↑ | Naert I, Gizani S, Vuylsteke M, van Steenberghe D. A randomised clinical trial on the influence of splinted and unsplinted oral implants in mandibular overdenture therapy. A 3-year report. → Clin Oral Investig. 1997 Jun;1(2):81–8. |
| 10. | ↑ | Batenburg RH, Raghoebar GM, Van Oort RP, Heijdenrijk K, Boering G. Mandibular overdentures supported by two or four endosteal implants. A prospective, comparative study. → Int J Oral Maxillofac Surg. 1998 Dec;27(6):435–9. |
| 11. | ↑ | Weinländer M, Piehslinger E, Krennmair G. Removable implant-prosthodontic rehabilitation of the edentulous mandible: five-year results of different prosthetic anchorage concepts. → Int J Oral Maxillofac Implants. 2010 May-Jun;25(3):589–97. |
| 13. | ↑ | Pozzi A, Tallarico M, Moy PK. Four-implant overdenture fully supported by a CAD-CAM titanium bar: a single-cohort prospective 1-year preliminary study. → J Prosthet Dent. 2016 Oct;116(4):516–23. |
| 15. | ↑ | Tallarico M, Meloni MS, Xhanari E, Canullo L. Three-year clinical and radiographic outcomes of patients treated according to the All-on-4 concept in the daily practice: a prospective observational study on implants and prosthesis survival rates and complications. → J Oral Science Rehabilitation. 2016 Jun;2(2):16–25. |
| 16. | ↑ | Abi Nader S, Eimar H, Momani M, Shang K, Daniel NG, Tamimi F. Plaque accumulation beneath maxillary All-on-4 implantsupported prostheses. → Clin Implant Dent Relat Res. 2015 Oct;17(5):932–7. |
| 17. | ↑ | Elm von E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. STROBE Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. → J Clin Epidemiol. 2008 Apr;61(4):344–9. |
| 18. | ↑ | Tallarico M, Vaccarella A, Marzi GC. Clinical and radiological outcomes of 1- versus 2-stage implant placement: 1-year results of a randomised clinical trial. → Eur J Oral Implantol. 2011 Spring;4(1):13–20. |
| 19. | ↑ | Pozzi A, Tallarico M, Mangani F, Barlattani A. Different implant impression techniques for edentulous patients treated with CAD/ CAM complete-arch prostheses: a randomised controlled trial reporting data at 3 year postloading. → Eur J Oral Implantol. 2013 Winter;6(4):325–40. |
| 20. | ↑ | Abduo J, Bennani V, Waddell N, Lyons K, Swain M. Assessing the fit of implant fixed prostheses: a critical review. → Int J Oral Maxillofac Implants. 2010 May-Jun;25(3):506–15. |
| 21. | ↑ | Eisenmann E, Mokabberi A, Walter MH, Freesmeyer WB. Improving the fit of implant-supported superstructures using the spark erosion technique. → Int J Oral Maxillofac Implants. 2004 Nov-Dec;19(6):810–8. |
| 22. | ↑ | Fitzpatrick B. Standard of care for the edentulous mandible: a systematic review. → J Prosthet Dent. 2006 Jan;95(1):71–8. |
| 23. | ↑ | Burns DR. Mandibular implant overdenture treatment: consensus and controversy. → J Prosthodont. 2000 Mar;9(1):37–46. |
| 24. | ↑ | Zitzmann NU, Marinello CP. Treatment plan for restoring the edentulous maxilla with implant-supported restorations: removable overdenture versus fixed partial denture design. → J Prosthet Dent. 1999 Aug;82(2):188–96. |
| 25. | ↑ | Jemt T, Book K, Linden B, Urde G. Failures and complications in 92 consecutively inserted overdentures supported by Brånemark implants in severely resorbed edentulous maxillae: a study from prosthetic treatment to first annual check-up. → Int J Oral Maxillofac Implants. 1992 Summer;7(2):162–7. |
| 26. | ↑ | Patzelt SB, Bahat O, Reynolds MA, Strub JR. The all-on-four treatment concept: a systematic review. → Clin Implant Dent Relat Res. 2014 Dec;16(6):836–55. |
| 27. | ↑ | Sadowsky SJ. Treatment considerations for maxillary implant overdentures: a systematic review. → J Prosthet Dent. 2007 Jun;97(6):340–8. |
| 28, 29. | ↑ | Tallarico M, Canullo L, Pisano M, Peñarrocha-Oltra D, Peñarrocha-Diago M, Meloni SM. An up to 7-year retrospective analysis of biologic and technical complication with the All-on-4 concept. → J Oral Implantol. 2016 Jun;42(3):265–71. |








Leave a Reply
Be the First to Comment!