Composition of platelet-rich plasma gel: A Western blot analysis
July 4, 2016 / Categories: Digital Dentistry, Implant Dentistry

Galindo Moreno, Pablo

Avila Ortiz, Gustavo

Torrecillas Martinez, Laura

Fernández Barbero, Juan Emilio

O’Valle Ravassa, Francisco

Wang, Hom-Lay
Platelet-rich plasma (PRP) gel is an autogenous blood-derived material that may be used as a regenerative agent of oral structures. The regenerative capacity of PRP is largely attributed to its composition, including many different growth factors. Thus far, no study has identified the molecular content of this gel. Therefore, it was the purpose of this study to assess the presence of different growth factors in PRP gel, using the Western blot technique.
Introduction
Tissue integrity and blood vessel repair are essential after destructive and reconstructive events, such as surgery, trauma and regenerative procedures. The seeking for and identification of reliable and safe techniques or therapeutic methods that would predictably enhance the regenerative capacity in damaged tissue has become a major focus of current research.
A large number of cells are involved in wound healing, including platelets, which play a crucial role in controlling coagulation and releasing growth factors and cytokines related to tissue regeneration. Platelet-derived products isolated from the patient’s own blood have been extensively studied and tested because platelets are considered a source of cytokines and growth factors, which amplify wound healing and tissue repair.1De Pascale MR, Sommese L, Casamassimi A, Napoli C. Platelet derivatives in regenerative medicine: an update. → Transfus Med Rev. 2015 Jan;29(1):52–61.
Platelet-rich plasma (PRP) offers much potential owing to its autogenous nature and a supposed molecular content. PRP was originally defined as a product with a high concentration of platelets, obtained from autologous blood, that contains different growth factors that may potentially influence cells involved in wound healing and bone regeneration.2Lu HH, Vo JM, Chin HS, Lin J, Cozin M, Tsay R, Eisig S, Landesberg R. Controlled delivery of platelet-rich plasma-derived growth factors for bone formation. → J Biomed Mater Res A. 2008 Sep;86(4):1128–36. Besides its adhesive and hemostatic properties, from a biological standpoint, the rationale for the use of PRP is rooted in the idea that regenerative advantages are obtained after the application of this product, given the modulating activity that is supposed to be exerted by molecules released from the α-granules, which are stored in the cytoplasm of platelets.3Marx RE, Carlson ER, Eichstaedt RM, Schimmele SR, Strauss JE, Georgeff KR. Platelet-rich plasma: growth factor enhancement for bone grafts. → Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998 Jun;85(6):638–46.’ 4Anitua E. Plasma rich in growth factors: preliminary results of use in the preparation of future sites for implants. → Int J Oral Maxillofac Implants. 1999 Jul-Aug;14(4):529–35. A wide variety of molecules with different biological roles are known to be contained in the different platelet granules, such as serotonin, coagulation factors, proteoglycans, membrane- associated proteins and different types of proteases.5De Pascale MR, Sommese L, Casamassimi A, Napoli C. Platelet derivatives in regenerative medicine: an update. → Transfus Med Rev. 2015 Jan;29(1):52–61.’ 6Anitua E, Andia I, Ardanza B, Nurden P, Nurden AT. Autologous platelets as a source of proteins for healing and tissue regeneration. → Thromb Haemost. 2004 Jan;91(1):4–15. However, some researchers believe that the activity of specific mitogenic/growth factors, concretely stored in the α-granules, is of major importance in regenerative events.7Marx RE. Platelet-rich plasma: evidence to support its use. → J Oral Maxillofac Surg. 2004 Apr;62(4):489–96.’ 8Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Gogly B. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part II: platelet-related biologic features. → Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006 Mar;101(3):e45–50. Growth factors, including those that have been classically associated with PRP, are included in a family of polypeptides of low molecular weight with a very short life span. Growth factors can modulate cell behavior, alter gene expression of target cells and ultimately lead to promotion of cell migration, proliferation, differentiation and eventually maturation.9Xie X, Zhang C, Tuan RS. Biology of platelet-rich plasma and its clinical application in cartilage repair. → Arthritis Res Ther. 2014 Feb;16(1):204. The growth factors that have been reported to be in PRP include vascular endothelial growth factor (VEGF), platelet-derived growth factor (PDGF), transforming growth factor-beta (TGF-β1), fibroblast growth factor (FGF), insulin-like growth factor-1 (IGF-1) and epidermal growth factor (EGF).10Lu HH, Vo JM, Chin HS, Lin J, Cozin M, Tsay R, Eisig S, Landesberg R. Controlled delivery of platelet-rich plasma-derived growth factors for bone formation. → J Biomed Mater Res A. 2008 Sep;86(4):1128–36.’ 11Marx RE. Platelet-rich plasma: evidence to support its use. → J Oral Maxillofac Surg. 2004 Apr;62(4):489–96.’ 12El-Sharkawy H, Kantarci A, Deady J, Hasturk H, Liu H, Alshahat M, Van Dyke TE. Platelet-rich plasma: growth factors and pro- and anti-inflammatory properties. → J Periodontol. 2007 Apr;78(4):661–9.
When PRP was introduced in dentistry, most of the knowledge that justified its attributed regenerative potential came from experimental animal models13Kim ES, Park EJ, Choung PH. Platelet concentration and its effect on bone formation in calvarial defects: an experimental study in rabbits. → J Prosthet Dent. 2001 Oct;86(4):428–33.’ 14Kim SG, Kim WK, Park JC, Kim HJ. A comparative study of osseointegration of Avana implants in a demineralized freeze-dried bone alone or with platelet-rich plasma. → J Oral Maxillofac Surg. 2002 Sep;60(9):1018–25. and several human case reports15Shanaman R, Filstein MR, Danesh-Meyer MJ. Localized ridge augmentation using GBR and platelet-rich plasma: case reports. → Int J Periodontics Restorative Dent. 2001 Aug;21(4):345–55.16Petrungaro PS. Treatment of the infected implant site using platelet-rich plasma. → Compend Contin Educ Dent. 2002 Apr;23(4):363–6, 368, 370 passim; quiz 378.17Froum SJ, Wallace SS, Tarnow DP, Cho SC. Effect of platelet-rich plasma on bone growth and osseointegration in human maxillary sinus grafts: three bilateral case reports. → Int J Periodontics Restorative Dent. 2002 Feb;22(1):45–53.18Thor A. Reconstruction of the anterior maxilla with platelet gel, autogenous bone, and titanium mesh: a case report. → Clin Implant Dent Relat Res. 2002 Oct;4(3):150–5.. Nowadays, clinical trials conducted to assess the clinical validity of PRP have shown controversial results, many of them advocating for no significant effect when PRP is used alone.19Powell CA, Bannister SR, Mackey SA, Maller SC, McDonnell HT, Deas DE. Periodontal wound healing with and without platelet-rich plasma: histologic observations and assessment of flap tensile strength. → J Periodontol. 2009 Jun;80(6):985–92.20Farina R, Bressan E, Taut A, Cucchi A, Trombelli L. Plasma rich in growth factors in human extraction sockets: a radiographic and histomorphometric study on early bone deposition. → Clin Oral Implants Res. 2013 Dec;24(12):1360–8.21Bezgin T, Yilmaz AD, Celik BN, Kolsuz ME, Sonmez H. Efficacy of platelet-rich plasma as a scaffold in regenerative endodontic treatment. → J Endod. 2015 Jan;41(1):36–44. However, it has been reported that the addition of PRP to bone substitutes promotes enhancement of osseointegration of dental implants, optimizing the expansion of new bone cells, and improvement of the aggregation and cohesiveness of particulate-based bone substitutes.22Plachokova AS, Nikolidakis D, Mulder J, Jansen JA, Creugers NH. Effect of platelet-rich plasma on bone regeneration in dentistry: a systematic review. → Clin Oral Implants Res. 2008 Jun;19(6):539–45.’ 23Forni F, Marzagalli M, Tesei P, Grassi A. Platelet gel: applications in dental regenerative surgery. → Blood Transfus. 2013 Jan;11(1):102–7. In order to understand how PRP works, it is important to know its structure and molecular composition.24Pietrzak WS, Eppley BL. Platelet rich plasma: biology and new technology. → J Craniofac Surg. 2005 Nov;16(6):1043–54. It is important to know whether the described factors are present in an amount that can be easily detectable and in what proportion of the population. However, only limited evidence is currently available. Hence, it was the aim of this study to conduct a qualitative analysis to screen the molecular composition of PRP.
Materials and methods
Preparation of PRP
Venous blood was obtained from 20 healthy volunteers (16 males and four females; mean age of 27.4), who gave their informed consent and met the following inclusion criteria after a complete medical history recording and examination: no medication taken in the last two weeks, no dental or intra-oral surgical treatment within the last month, and no vaccine received and no infection history within the last three months. Briefly, 20 cm3 of blood was drawn per patient and 5 cm3 placed into each of four Vacutainer tubes (Becton Dickinson, Oxford, U.K.), which contained 0.1 cm3 of 3.8% (w/v) sodium citrate. In order to minimize platelet activation during blood collection, a 19-gauge butterfly needle with a light tourniquet was used and the first 2 mL of blood was discarded. For the preparation of the PRP, a modification of the original procedure proposed by Anitua in 1999 was followed.25Anitua E. Plasma rich in growth factors: preliminary results of use in the preparation of future sites for implants. → Int J Oral Maxillofac Implants. 1999 Jul-Aug;14(4):529–35. Immediately after collection, the tubes were placed in a centrifuge machine to spin at 1,500 rpm for 7 min in order to separate the blood fractions. In order to produce PRP, 500 mL from the volume of plasma situated just over the top of the red fraction was collected from every sample. To each 500 mL of plasma, 250 mL of calcium chloride was added. Finally, the tubes were placed in a 37 ºC warm water bath for 20 min to accelerate the formation of a PRP gel. The remaining contents of the tubes was discarded.
Monoclonal and polyclonal antibodies
The Western blot technique was performed using monoclonal antibodies for the selected platelet growth factors: anti-VEGF (C-1: sc-7269; Santa Cruz Biotechnology, Santa Cruz, Calif., U.S.), anti-PDGF-A (E-10; sc-9974; Santa Cruz Biotechnology), anti-human TGF-ß1 (Clone 9016.2; Sigma-Aldrich, St. Louis, Mo., U.S.), anti-human IGF-1 Goat (Sigma-Aldrich), anti-human bFGF (Clone FB-8; Sigma-Aldrich) and anti-human EGF (Clone EGF-10; Sigma-Aldrich). Fluorochrome- marked polyclonal immunoglobulin-G antibodies able to bind the previously mentioned antibodies were purchased from Santa Cruz Biotechnology to be used as secondary antibodies.
Western blot technique
Gels for electrophoresis (12% SDS-PAGE) were initially prepared for each experiment. Final samples consisting of a volume of 15 mL of PRP clot, previously diluted in a sample buffer (at a proportion of 1 mg/mL), were properly identified and placed on each well of the electrophoresis gels. The proteins were electrophoretically run at a rate of 60 V and 45 mA for 2 h, using the Power- Pac HC electrophoresis kit (Bio-Rad, Laboratories, Hercules, Calif., U.S.). Transference of the proteins located in the running gel was performed using a Trans-Blot SD device (Bio-Rad), at 25 V/60 mA for 50 min. Once the transference to nitrocellulose membranes, designed for protein transference, had been completed, specimens were submerged in 20 mL of blocking suspension (5 mg of fat-free powder milk diluted in 100 mL of 1 × TBS) for 60 min, at room temperature. After that, the membranes were incubated with the mentioned specific monoclonal antibodies for different growth factors in agitation, for 24 h at 4 °C. Three 5 min washes using a washing solution (0.5 mL of 0.1% TWEEN 20 in 500 mL of 1 × TBS) were performed prior to the incubation of the membranes with the secondary antibodies, for 2 h at room temperature. Finally, the membranes received three 5 min washes (0.5 mL of 0.1% TWEEN 20 in 500 mL of 1 × TBS), and they were developed and scanned. Bands for each sample were assessed and assigned to three levels of intensity: band not visible (–); band visible but not solid (+/–); and solid positive band (+).
Results
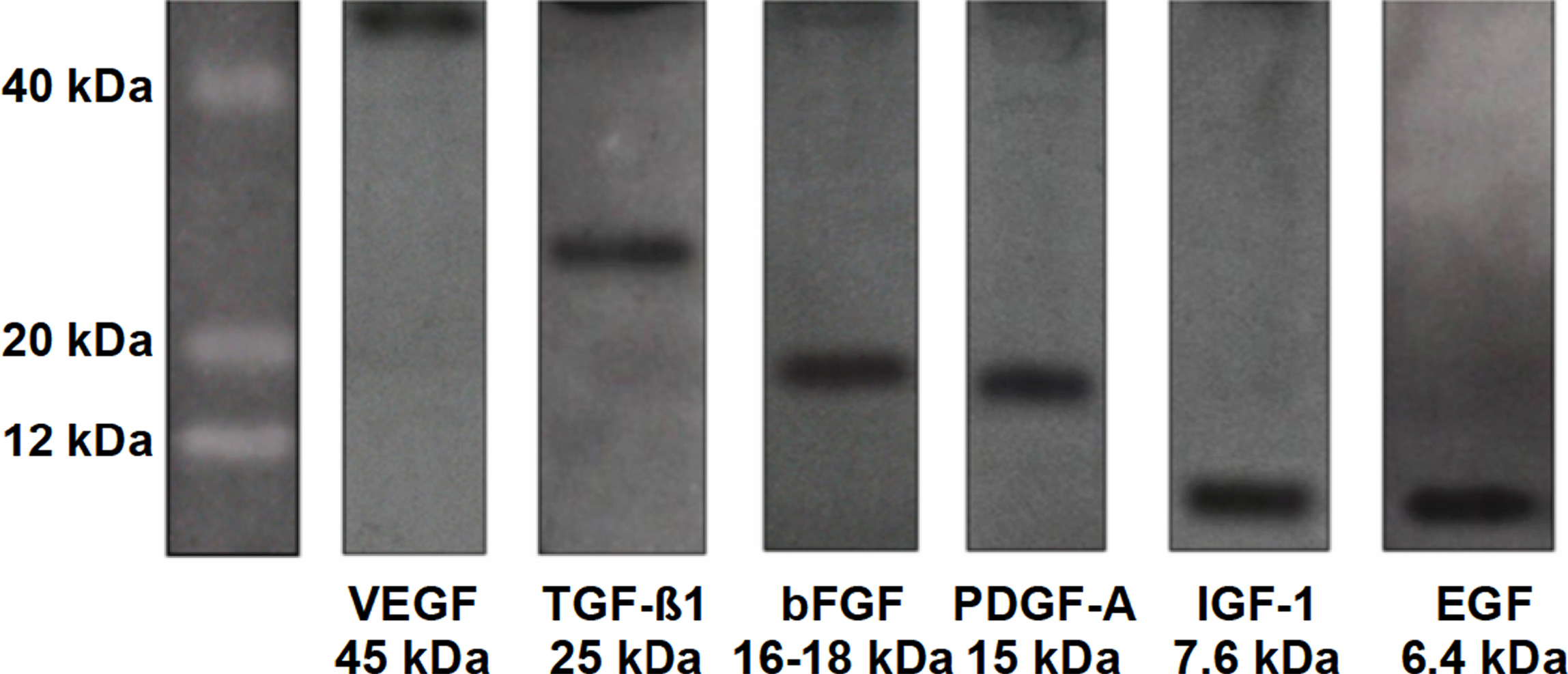
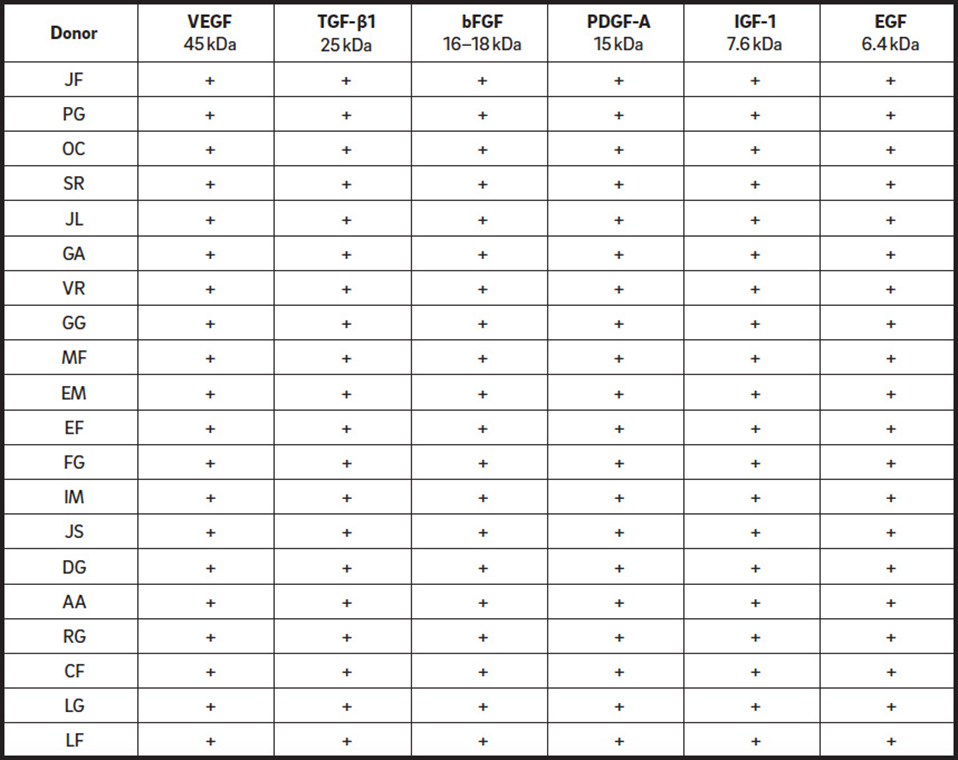
In this qualitative analysis, all growth factors under study (VEGF, PDGF-A, TGF-β1, bFGF, IGF- 1 and EGF) were present in all of the patients (Table 1). The bands observed as positive after developing the membrane were located at the presumed molecular weight for each of the factors: VEGF at 45 kDa, TGF-β1 at 25 kDa, bFGF at 17 kDa, PDGF-A at 15 kDa, IGF-1 at 7.6 kDa and EGF at 6.4 kDa (Fig. 1).
Discussion
PRP has been suggested to be a novel agent that could promote not only hard-tissue regeneration26Marx RE, Carlson ER, Eichstaedt RM, Schimmele SR, Strauss JE, Georgeff KR. Platelet-rich plasma: growth factor enhancement for bone grafts. → Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998 Jun;85(6):638–46. but also soft-tissue healing.27Man D, Plosker H, Winland-Brown JE. The use of autologous platelet-rich plasma (platelet gel) and autologous platelet-poor plasma (fibrin glue) in cosmetic surgery. → Plast Reconstr Surg. 2001 Jan;107(1):229–37; discussion 238–9. Although controversy exists regarding its ability to promote regeneration, especially in hard tissue,28Farina R, Bressan E, Taut A, Cucchi A, Trombelli L. Plasma rich in growth factors in human extraction sockets: a radiographic and histomorphometric study on early bone deposition. → Clin Oral Implants Res. 2013 Dec;24(12):1360–8.’ 29Thor A, Wannfors K, Sennerby L, Rasmusson L. Reconstruction of the severely resorbed maxilla with autogenous bone, platelet-rich plasma, and implants: 1-year results of a controlled prospective 5-year study. → Clin Implant Dent Relat Res. 2005 Oct;7(4):209–20.’ 30Raghoebar GM, Schortinghuis J, Liem RS, Ruben JL, Van Der Wal JE, Vissink A. Does platelet-rich plasma promote remodeling of autologous bone grafts used for augmentation of the maxillary sinus floor? → Clin Oral Implants Res. 2005 Jun;16(3):349–56. many clinicians remain loyal to its clinical usage. In order to enhance understanding of PRP, our research group has focused on analyzing the structure and composition of PRP gel using flow cytometry and the scanning electron microscope.31Fernández-Barbero JE, Galindo-Moreno P, Avila-Ortiz G, Caba O, Sánchez-Fernández E, Wang HL. Flow cytometric and morphological characterization of platelet-rich plasma gel. → Clin Oral Implants Res. 2006 Dec;17(6):687–93. Our results have shown PRP’s microstructural composition, essentially constituted by fibrin in relation to the different cellular elements in the clot, identified as largely platelets in different stages of activation.
Following the line traced by those previous findings, our group has designed a further in vitro study to determine the presence of different growth factors known to be present in the α-granules of the platelets in PRP gel samples.32Rendu F, Brohard-Bohn B. The platelet release reaction: granules’ constituents, secretion and functions. → Platelets. 2001 Aug;12(5):261–73. Results obtained from the present study indicate that PRP gel contains the six tested growth factors: VEGF, PDGF, TGF-β1, FGF, IGF-1 and EGF. These growth factors have been known for their influence at different stages of the healing processes.33Xie X, Zhang C, Tuan RS. Biology of platelet-rich plasma and its clinical application in cartilage repair. → Arthritis Res Ther. 2014 Feb;16(1):204.’ 34Plachokova AS, Nikolidakis D, Mulder J, Jansen JA, Creugers NH. Effect of platelet-rich plasma on bone regeneration in dentistry: a systematic review. → Clin Oral Implants Res. 2008 Jun;19(6):539–45. Basically, growth factors are lowweighted molecules produced and released by many different cell types under variable stimuli and play a determinant role in the development and maturation of different tissues in mammals. For instance, VEGF is an important regulator of angiogenic processes, increasing vessel permeability and contributing essentially to neoangiogenesis. Its presence in the clot of PRP can partially justify the positive outcomes obtained in some studies regarding the beneficial effect of PRP on capillary growth in soft-tissue wound healing.35Lindeboom JA, Mathura KR, Aartman IH, Kroon FH, Milstein DM, Ince C. Influence of the application of platelet-enriched plasma in oral mucosal wound healing. → Clin Oral Implants Res. 2007 Feb;18(1):133–9. Several in vitro and animal studies have illustrated the modulating effect that growth factors exert on different cell types. PDGF is primarily responsible for tissue healing and has been shown to induce proliferation of gingival fibroblasts and osteoblasts36Zhang L, Leeman E, Carnes DC, Graves DT. Human osteoblasts synthesize and respond to platelet-derived growth factor. → Am J Physiol. 1991 Aug;261(2):C348–54. and adherence of periodontal ligament cells to root surfaces.37Gamal AY, Mailhot JM. The effect of local delivery of PDGF-BB on attachment of human periodontal ligament fibroblasts to periodontitis-affected root surfaces—in vitro. → J Clin Periodontol. 2000 May;27(5):347–53. TGF-β1 is essential for normal tissue remodeling and wound healing; it is chemotactic for human fibroblasts,38Postlethwaite AE, Keski-Oja J, Moses HL, Kang AH. Stimulation of the chemotactic migration of human fibroblasts by transforming growth factor β. → J Exp Med. 1987 Jan;165(1):251–6. enhances the proliferation and differentiation of osteoblasts,39Centrella M, McCarthy TL, Canalis E. Transforming growth factor β is a bifunctional regulator of replication and collagen synthesis in osteoblast-enriched cell cultures from fetal rat bone. → J Biol Chem. 1987 Feb;262(6):2869–74.40Mundy GR, Boyce B, Hughes D, Wright K, Bonewald L, Dallas S, Harris S, Ghosh-Choudhury N, Chen D, Dunstan C, Izbicka E, Yoneda T. The effects of cytokines and growth factors on osteoblastic cells. → Bone. 1995 Aug;17(2 Suppl):S71–75.41Graham S, Leonidou A, Lester M, Heliotis M, Mantalaris A, Tsiridis E. Investigating the role of PDGF as a potential drug therapy in bone formation and fracture healing. → Expert Opin Investig Drugs. 2009 Nov;18(11):1633–54. and intervenes in angiogenesis and immunomodulation.42Ghosh D, Lili L, McGrail DJ, Matyunina LV, McDonald JF, Dawson MR. Integral role of platelet-derived growth factor in mediating transforming growth factor-β1-dependent mesenchymal stem cell stiffening. → Stem Cells Dev. 2014 Feb;23(3):245–61. BFGF induces stimulation of periodontal ligament cell proliferation, osteoblastic cell proliferation and growth and fibroblasts, and plays a role in angiogenesis.43Sonmez AB, Castelnuovo J. Applications of basic fibroblastic growth factor (FGF-2, bFGF) in dentistry. → Dent Traumatol. 2014 Apr;30(2):107–11.44Terranova VP, Odziemiec C, Tweden KS, Spadone DP. Repopulation of dentin surfaces by periodontal ligament cells and endothelial cells: effect of basic fibroblast growth factor. → J Periodontol. 1989 Jun;60(6):293–301.45Cross MJ, Claesson-Welsh L. FGF and VEGF function in angiogenesis: signalling pathways, biological responses and therapeutic inhibition. → Trends Pharmacol Sci. 2001 Apr;22(4):201–7. IGF-1, also known as somatomedin, is a mediator in the activity of growth hormone46Laron Z. Clinical use of somatomedin-1: yes or no? → Paediatr Drugs. 1999 Jul-Sep;1(3):155–9. and a positive regulator of cell proliferation and differentiation for most cell types.47Ren J, Anversa P. The insulin-like growth factor I system: physiological and pathophysiological implication in cardiovascular diseases associated with metabolic syndrome. → Biochem Pharmacol. 2015 Feb;93(4):409–17. EGF enhances the proliferation of keratinocytes48Brown GL, Nanney LB, Griffen J, Cramer AB, Yancey JM, Curtsinger LJ 3rd, Holtzin L, Schultz GS, Jurkiewicz MJ, Lynch JB. Enhancement of wound healing by topical treatment with epidermal growth factor. → N Engl J Med. 1989 Jul;321(2):76–9. and is implicated in epithelialization, wound contraction and remodeling.49Brown GL, Curtsinger LJ, White M, Mitchell RO, Pietsch J, Nordquist R, von Fraunhofer A, Schultz GS. Acceleration of tensile strength of incisions treated with EGF and TGF-β. → Ann Surg. 1988 Dec;208(6):788–94.
Thus far, the majority of studies reporting detection of one or some of the previously mentioned growth factors in PRP samples have been conducted on nonclotted samples, without any platelet activator added.50Marx RE, Carlson ER, Eichstaedt RM, Schimmele SR, Strauss JE, Georgeff KR. Platelet-rich plasma: growth factor enhancement for bone grafts. → Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998 Jun;85(6):638–46.,51Zimmermann R, Jakubietz R, Jakubietz M, Strasser E, Schlegel A, Wiltfang J, Eckstein R. Different preparation methods to obtain platelet components as a source of growth factors for local application. → Transfusion. 2001 Oct;41(10):1217–24.52Weibric G, Buch RS, Kleis WK, Hafner G, Hitzler WE, Wagner W. Quantification of thrombocyte growth factors in platelet concentrates produced by discontinuous cell separation. → Growth Factors. 2002 Jun;20(2):93–7.53Weibrich G, Kleis WK, Buch R, Hitzler WE, Hafner G. The Harvest Smart PReP™ system versus the Friadent-Schütze platelet-rich plasma kit. → Clin Oral Implants Res. 2003 Apr;14(2):233–9.54Eppley BL, Woodell JE, Higgins J. Platelet quantification and growth factor analysis from platelet-rich plasma: implications for wound healing. → Plast Reconstr Surg. 2004 Nov;114(6):1502–8. In our opinion, direct analysis of the presence of growth factors in PRP gel would provide a more accurate idea regarding which are the bioactive constituents of PRP gel.
El-Sharkawy et al. performed a similar study based on a different technique, enzyme-linked immunosorbent assay (ELISA), and the same growth factor content of PRP was found.55El-Sharkawy H, Kantarci A, Deady J, Hasturk H, Liu H, Alshahat M, Van Dyke TE. Platelet-rich plasma: growth factors and pro- and anti-inflammatory properties. → J Periodontol. 2007 Apr;78(4):661–9. They quantified platelet and growth factor levels. PDGF, TGF-β1, IGF-1, EGF, VEGF and bFGF were also identified in their PRP samples. They attributed the biological properties of these growth factors, such as proliferation of fibroblasts and periodontal ligament cells and extracellular matrix formation, to PRP. Lu et al. also used the same technique, ELISA, and they identified and quantified PRP growth factors released (PDGF, TGF-β1 and IGF-1), obtaining similar results, although no search for EGF, VEGF or bFGF was conducted.56Lu HH, Vo JM, Chin HS, Lin J, Cozin M, Tsay R, Eisig S, Landesberg R. Controlled delivery of platelet-rich plasma-derived growth factors for bone formation. → J Biomed Mater Res A. 2008 Sep;86(4):1128–36.
Despite the contribution of our findings to the understanding of PRP biology, they also raise more questions that need to be addressed. The identification of these growth factors in PRP gel only suggests their presence in the clot, without providing evidence supporting its biological benefit after its clinical usage, especially for regenerative approaches. Growth factors are proteins that, once released from the producer cell, exert a very localized action at specific ratios,57Vilček J. The cytokines: an overview. In: Thomson AW, Lotze MT, editors. → The cytokine handbook. Vol. 1. Avon (MA): Academic Press; 2003. p. 3–18. owing to their short life span. They are labile molecules highly susceptible to denaturalization mediated by proteases present in the wound site and to phagocytosis and might even become solubilized in the carrier.58Giannobile WV. Periodontal tissue engineering by growth factors. → Bone. 1996 Jul;19(1 Suppl):S23–37. These undesirable events usually lead to the inactivation or annulment of the biological properties of these mediators. For instance, PDGF cannot be detected in circulating blood in normal conditions, and when it is intravenously injected, its life span is around 2 min.59Nimni ME. Polypeptide growth factors: targeted delivery systems. → Biomaterials. 1997 Sep;18(18):1201–25. This lack of long-term activity associated with the short half-life of this platelet growth factor may require repeated applications over time to maintain their therapeutic effect.
Both the vehicle and concentration (dose) of biological mediators, such as platelet growth factors, may be critical factors to consider when seeking to achieve controlled modulation of cellular events in the desired time interval.60Hokugo A, Ozeki M, Kawakami O, Sugimoto K, Mushimoto K, Morita S, Tabata Y. Augmented bone regeneration activity of platelet-rich plasma by biodegradable gelatin hydrogel. → Tissue Eng. 2005 Jul-Aug;11(7-8):1224–33. However, it has to be taken into consideration that there is no currently available information about the optimal dosages of PRP needed to achieve the highest effectiveness.61De Pascale MR, Sommese L, Casamassimi A, Napoli C. Platelet derivatives in regenerative medicine: an update. → Transfus Med Rev. 2015 Jan;29(1):52–61.
It is also important to note that the technique used in this study for the detection of growth factors, Western blotting, allows detection of the presence of a determined protein in a sample by highly specific binding of antibodies to epitopes of that polypeptide. However, it is not possible to ultimately determine whether the target protein is biologically active and therefore able to exert its effect when applied to a wound. This fact, along with the arguments discussed before, moves us to reason that the beneficial effects obtained after application of autologous PRP gel may not be mediated only by the action of growth factors.
Considering this data, it is logical to outline several questions and doubts regarding the variable amount of growth factors, presenting a true ability to interact with the environment, that may be released from the PRP gel sample that is clinically applied. Are those growth factors the exclusive or major mediators responsible for a change in the biological conditions that lead to an improvement in tissue regeneration? Does the fibrillar component of the clot have a role in modulating the biological response that permits a better clinical response? Or, is it a synergistic effect between the fibrillar scaffold and different molecular components of blood plasma, among which growth factors are present, that induces those beneficial effects?
Understanding the role of each component of PRP gel in wound-healing events and the optimal concentration of molecules with the capacity of modulating these processes remains one of the major challenges for researchers in this field of tissue engineering. In order to address those questions, further in vitro and in vivo studies seeking to determine the physical interaction of PRP elements with cell types present in the craniofacial surgical field and its impact on cell proliferation and differentiation are needed.
Competing interests
The authors do not have any financial interests, either directly or indirectly, in the products listed in the study.
Acknowledgments
This article was supported partially by Research Group #CTS-583 (Junta de Andalucía, Spain).
References
| 1, 5, 61. | ↑ | De Pascale MR, Sommese L, Casamassimi A, Napoli C. Platelet derivatives in regenerative medicine: an update. → Transfus Med Rev. 2015 Jan;29(1):52–61. |
| 2, 10, 56. | ↑ | Lu HH, Vo JM, Chin HS, Lin J, Cozin M, Tsay R, Eisig S, Landesberg R. Controlled delivery of platelet-rich plasma-derived growth factors for bone formation. → J Biomed Mater Res A. 2008 Sep;86(4):1128–36. |
| 3, 26, 50. | ↑ | Marx RE, Carlson ER, Eichstaedt RM, Schimmele SR, Strauss JE, Georgeff KR. Platelet-rich plasma: growth factor enhancement for bone grafts. → Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998 Jun;85(6):638–46. |
| 4, 25. | ↑ | Anitua E. Plasma rich in growth factors: preliminary results of use in the preparation of future sites for implants. → Int J Oral Maxillofac Implants. 1999 Jul-Aug;14(4):529–35. |
| 6. | ↑ | Anitua E, Andia I, Ardanza B, Nurden P, Nurden AT. Autologous platelets as a source of proteins for healing and tissue regeneration. → Thromb Haemost. 2004 Jan;91(1):4–15. |
| 7, 11. | ↑ | Marx RE. Platelet-rich plasma: evidence to support its use. → J Oral Maxillofac Surg. 2004 Apr;62(4):489–96. |
| 8. | ↑ | Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Gogly B. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part II: platelet-related biologic features. → Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006 Mar;101(3):e45–50. |
| 9, 33. | ↑ | Xie X, Zhang C, Tuan RS. Biology of platelet-rich plasma and its clinical application in cartilage repair. → Arthritis Res Ther. 2014 Feb;16(1):204. |
| 12, 55. | ↑ | El-Sharkawy H, Kantarci A, Deady J, Hasturk H, Liu H, Alshahat M, Van Dyke TE. Platelet-rich plasma: growth factors and pro- and anti-inflammatory properties. → J Periodontol. 2007 Apr;78(4):661–9. |
| 13. | ↑ | Kim ES, Park EJ, Choung PH. Platelet concentration and its effect on bone formation in calvarial defects: an experimental study in rabbits. → J Prosthet Dent. 2001 Oct;86(4):428–33. |
| 14. | ↑ | Kim SG, Kim WK, Park JC, Kim HJ. A comparative study of osseointegration of Avana implants in a demineralized freeze-dried bone alone or with platelet-rich plasma. → J Oral Maxillofac Surg. 2002 Sep;60(9):1018–25. |
| 15. | ↑ | Shanaman R, Filstein MR, Danesh-Meyer MJ. Localized ridge augmentation using GBR and platelet-rich plasma: case reports. → Int J Periodontics Restorative Dent. 2001 Aug;21(4):345–55. |
| 16. | ↑ | Petrungaro PS. Treatment of the infected implant site using platelet-rich plasma. → Compend Contin Educ Dent. 2002 Apr;23(4):363–6, 368, 370 passim; quiz 378. |
| 17. | ↑ | Froum SJ, Wallace SS, Tarnow DP, Cho SC. Effect of platelet-rich plasma on bone growth and osseointegration in human maxillary sinus grafts: three bilateral case reports. → Int J Periodontics Restorative Dent. 2002 Feb;22(1):45–53. |
| 18. | ↑ | Thor A. Reconstruction of the anterior maxilla with platelet gel, autogenous bone, and titanium mesh: a case report. → Clin Implant Dent Relat Res. 2002 Oct;4(3):150–5. |
| 19. | ↑ | Powell CA, Bannister SR, Mackey SA, Maller SC, McDonnell HT, Deas DE. Periodontal wound healing with and without platelet-rich plasma: histologic observations and assessment of flap tensile strength. → J Periodontol. 2009 Jun;80(6):985–92. |
| 20, 28. | ↑ | Farina R, Bressan E, Taut A, Cucchi A, Trombelli L. Plasma rich in growth factors in human extraction sockets: a radiographic and histomorphometric study on early bone deposition. → Clin Oral Implants Res. 2013 Dec;24(12):1360–8. |
| 21. | ↑ | Bezgin T, Yilmaz AD, Celik BN, Kolsuz ME, Sonmez H. Efficacy of platelet-rich plasma as a scaffold in regenerative endodontic treatment. → J Endod. 2015 Jan;41(1):36–44. |
| 22, 34. | ↑ | Plachokova AS, Nikolidakis D, Mulder J, Jansen JA, Creugers NH. Effect of platelet-rich plasma on bone regeneration in dentistry: a systematic review. → Clin Oral Implants Res. 2008 Jun;19(6):539–45. |
| 23. | ↑ | Forni F, Marzagalli M, Tesei P, Grassi A. Platelet gel: applications in dental regenerative surgery. → Blood Transfus. 2013 Jan;11(1):102–7. |
| 24. | ↑ | Pietrzak WS, Eppley BL. Platelet rich plasma: biology and new technology. → J Craniofac Surg. 2005 Nov;16(6):1043–54. |
| 27. | ↑ | Man D, Plosker H, Winland-Brown JE. The use of autologous platelet-rich plasma (platelet gel) and autologous platelet-poor plasma (fibrin glue) in cosmetic surgery. → Plast Reconstr Surg. 2001 Jan;107(1):229–37; discussion 238–9. |
| 29. | ↑ | Thor A, Wannfors K, Sennerby L, Rasmusson L. Reconstruction of the severely resorbed maxilla with autogenous bone, platelet-rich plasma, and implants: 1-year results of a controlled prospective 5-year study. → Clin Implant Dent Relat Res. 2005 Oct;7(4):209–20. |
| 30. | ↑ | Raghoebar GM, Schortinghuis J, Liem RS, Ruben JL, Van Der Wal JE, Vissink A. Does platelet-rich plasma promote remodeling of autologous bone grafts used for augmentation of the maxillary sinus floor? → Clin Oral Implants Res. 2005 Jun;16(3):349–56. |
| 31. | ↑ | Fernández-Barbero JE, Galindo-Moreno P, Avila-Ortiz G, Caba O, Sánchez-Fernández E, Wang HL. Flow cytometric and morphological characterization of platelet-rich plasma gel. → Clin Oral Implants Res. 2006 Dec;17(6):687–93. |
| 32. | ↑ | Rendu F, Brohard-Bohn B. The platelet release reaction: granules’ constituents, secretion and functions. → Platelets. 2001 Aug;12(5):261–73. |
| 35. | ↑ | Lindeboom JA, Mathura KR, Aartman IH, Kroon FH, Milstein DM, Ince C. Influence of the application of platelet-enriched plasma in oral mucosal wound healing. → Clin Oral Implants Res. 2007 Feb;18(1):133–9. |
| 36. | ↑ | Zhang L, Leeman E, Carnes DC, Graves DT. Human osteoblasts synthesize and respond to platelet-derived growth factor. → Am J Physiol. 1991 Aug;261(2):C348–54. |
| 37. | ↑ | Gamal AY, Mailhot JM. The effect of local delivery of PDGF-BB on attachment of human periodontal ligament fibroblasts to periodontitis-affected root surfaces—in vitro. → J Clin Periodontol. 2000 May;27(5):347–53. |
| 38. | ↑ | Postlethwaite AE, Keski-Oja J, Moses HL, Kang AH. Stimulation of the chemotactic migration of human fibroblasts by transforming growth factor β. → J Exp Med. 1987 Jan;165(1):251–6. |
| 39. | ↑ | Centrella M, McCarthy TL, Canalis E. Transforming growth factor β is a bifunctional regulator of replication and collagen synthesis in osteoblast-enriched cell cultures from fetal rat bone. → J Biol Chem. 1987 Feb;262(6):2869–74. |
| 40. | ↑ | Mundy GR, Boyce B, Hughes D, Wright K, Bonewald L, Dallas S, Harris S, Ghosh-Choudhury N, Chen D, Dunstan C, Izbicka E, Yoneda T. The effects of cytokines and growth factors on osteoblastic cells. → Bone. 1995 Aug;17(2 Suppl):S71–75. |
| 41. | ↑ | Graham S, Leonidou A, Lester M, Heliotis M, Mantalaris A, Tsiridis E. Investigating the role of PDGF as a potential drug therapy in bone formation and fracture healing. → Expert Opin Investig Drugs. 2009 Nov;18(11):1633–54. |
| 42. | ↑ | Ghosh D, Lili L, McGrail DJ, Matyunina LV, McDonald JF, Dawson MR. Integral role of platelet-derived growth factor in mediating transforming growth factor-β1-dependent mesenchymal stem cell stiffening. → Stem Cells Dev. 2014 Feb;23(3):245–61. |
| 43. | ↑ | Sonmez AB, Castelnuovo J. Applications of basic fibroblastic growth factor (FGF-2, bFGF) in dentistry. → Dent Traumatol. 2014 Apr;30(2):107–11. |
| 44. | ↑ | Terranova VP, Odziemiec C, Tweden KS, Spadone DP. Repopulation of dentin surfaces by periodontal ligament cells and endothelial cells: effect of basic fibroblast growth factor. → J Periodontol. 1989 Jun;60(6):293–301. |
| 45. | ↑ | Cross MJ, Claesson-Welsh L. FGF and VEGF function in angiogenesis: signalling pathways, biological responses and therapeutic inhibition. → Trends Pharmacol Sci. 2001 Apr;22(4):201–7. |
| 46. | ↑ | Laron Z. Clinical use of somatomedin-1: yes or no? → Paediatr Drugs. 1999 Jul-Sep;1(3):155–9. |
| 47. | ↑ | Ren J, Anversa P. The insulin-like growth factor I system: physiological and pathophysiological implication in cardiovascular diseases associated with metabolic syndrome. → Biochem Pharmacol. 2015 Feb;93(4):409–17. |
| 48. | ↑ | Brown GL, Nanney LB, Griffen J, Cramer AB, Yancey JM, Curtsinger LJ 3rd, Holtzin L, Schultz GS, Jurkiewicz MJ, Lynch JB. Enhancement of wound healing by topical treatment with epidermal growth factor. → N Engl J Med. 1989 Jul;321(2):76–9. |
| 49. | ↑ | Brown GL, Curtsinger LJ, White M, Mitchell RO, Pietsch J, Nordquist R, von Fraunhofer A, Schultz GS. Acceleration of tensile strength of incisions treated with EGF and TGF-β. → Ann Surg. 1988 Dec;208(6):788–94. |
| 51. | ↑ | Zimmermann R, Jakubietz R, Jakubietz M, Strasser E, Schlegel A, Wiltfang J, Eckstein R. Different preparation methods to obtain platelet components as a source of growth factors for local application. → Transfusion. 2001 Oct;41(10):1217–24. |
| 52. | ↑ | Weibric G, Buch RS, Kleis WK, Hafner G, Hitzler WE, Wagner W. Quantification of thrombocyte growth factors in platelet concentrates produced by discontinuous cell separation. → Growth Factors. 2002 Jun;20(2):93–7. |
| 53. | ↑ | Weibrich G, Kleis WK, Buch R, Hitzler WE, Hafner G. The Harvest Smart PReP™ system versus the Friadent-Schütze platelet-rich plasma kit. → Clin Oral Implants Res. 2003 Apr;14(2):233–9. |
| 54. | ↑ | Eppley BL, Woodell JE, Higgins J. Platelet quantification and growth factor analysis from platelet-rich plasma: implications for wound healing. → Plast Reconstr Surg. 2004 Nov;114(6):1502–8. |
| 57. | ↑ | Vilček J. The cytokines: an overview. In: Thomson AW, Lotze MT, editors. → The cytokine handbook. Vol. 1. Avon (MA): Academic Press; 2003. p. 3–18. |
| 58. | ↑ | Giannobile WV. Periodontal tissue engineering by growth factors. → Bone. 1996 Jul;19(1 Suppl):S23–37. |
| 59. | ↑ | Nimni ME. Polypeptide growth factors: targeted delivery systems. → Biomaterials. 1997 Sep;18(18):1201–25. |
| 60. | ↑ | Hokugo A, Ozeki M, Kawakami O, Sugimoto K, Mushimoto K, Morita S, Tabata Y. Augmented bone regeneration activity of platelet-rich plasma by biodegradable gelatin hydrogel. → Tissue Eng. 2005 Jul-Aug;11(7-8):1224–33. |



Leave a Reply
Be the First to Comment!