Implant-supported mandibular complete fixed prosthesis with conometric retention after 3 years of functional loading
July 6, 2018 / Categories: Digital Dentistry, Implant Dentistry

Bressan, Eriberto

Stocchero, Michele

Buso, Maddalena

Stellini, Edoardo

Ludovichetti, Francesco Saverio

Lops, Diego
Abstract
Objective
The aim of the study was to assess the clinical performance of implant-supported mandibular complete fixed prostheses with conometric retention after 3 years of functional loading.
Materials and methods
In this retrospective study, patients treated with implant-supported mandibular complete fixed prostheses with conometric retention were considered. Standardized radiographic examinations were performed to assess the marginal bone. Radiographs were acquired at the time of prosthesis insertion and at the 3-year follow-up, and marginal bone loss was calculated. The occurrence of implant failures, and biological and technical complications was registered.
Results
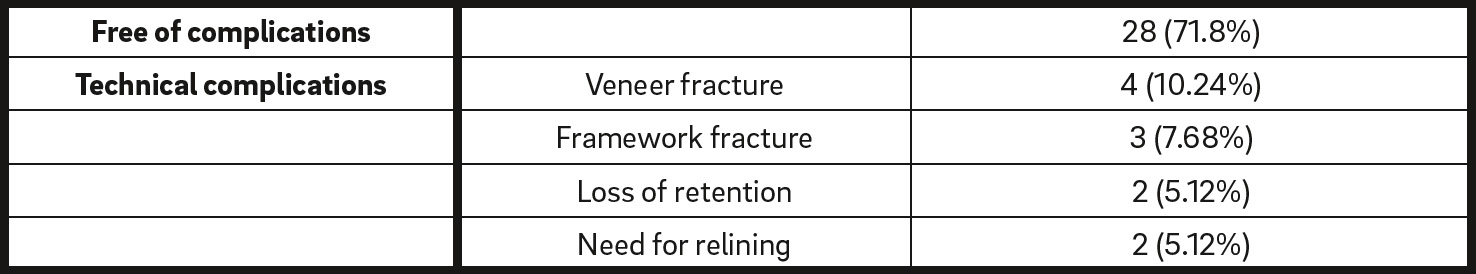
Thirty-nine patients were selected. At the 3-year follow-up, 134 out of the 160 placed implants did not show any marginal bone loss and 4 of them had been lost. The percentage of restorations free of technical complications was 71.8% during the entire follow-up period. Complications that occurred in restorations were as follows: veneer fracture (n = 4), framework fracture (n = 3), loss of retention (n = 2) and need for relining (n = 2). Mucositis was recorded in 1 patient and it was successfully treated.
Conclusion
The clinical performance of implant-supported mandibular complete fixed prostheses with conometric retention after 3 years of functional loading showed a low rate of marginal bone loss and technical complications. Owing to the easy retrievability, all complications were successfully treated.
Keywords
Fixed prostheses; dental implants; conometric retention; edentulous mandible.
Introduction
The rehabilitation of edentate patients with the use of implant-supported fixed dental prostheses (IFDPs) has shown high long-term survival rates, comparable to those of tooth-borne restorations.1Pjetursson BE, Asgeirsson AG, Zwahlen M, Sailer I. Improvements in implant dentistry over the last decade: comparison of survival and complication rates in older and newer publications. → Int J Oral Maxillofac Implants. 2014;29 Suppl:308–24. The clinical success, however, depends on the extent of biological and technical complications occurring throughout the period of function.2Sailer I, Mühlemann S, Zwahlen M, Hämmerle CH, Schneider D. Cemented and screw-retained implant reconstructions: a systematic review of the survival and complication rates. → Clin Oral Implants Res. 2012 Oct;23 Suppl 6:163–201. According to a systematic review, the patient-centered estimated 5-year complication rate for IFDPs was 33.6%.3Pjetursson BE, Thoma D, Jung R, Zwahlen M, Zembic A. A systematic review of the survival and complication rates of implant-supported fixed dental prostheses (FDPs) after a mean observation period of at least 5 years. → Clin Oral Implants Res. 2012 Oct;23 Suppl 6:22–38. Such issues can be better addressed when restorations can be easily removed. Thus, a remarkable research effort has been dedicated to protocols with enhanced retrievability.4Proussaefs P, AlHelal A. The combination prosthesis: a digitally designed retrievable cement- and screw-retained implant-supported prosthesis. → J Prosthet Dent. 2018 Apr;119(4):535–9. Epub 2017 Sep 18.
One of the major topics of discussion among researchers and clinicians is the type of fixation between the implant and the prosthesis. Such connection is commonly provided by means of screws or cement. None of the fixation methods has been found to be clearly advantageous over the other.5Shadid R, Sadaqa N. A comparison between screw- and cement-retained implant prostheses. A literature review. → J Oral Implantol. 2012 Jun;38(3):298–307. Moreover, they typically show some drawbacks. Screw-retained prostheses tend to experience more technical complications, such as screw loosening and fractures, while cemented restorations exhibit more biological complications, such as implant loss and marginal bone loss.6Sailer I, Mühlemann S, Zwahlen M, Hämmerle CH, Schneider D. Cemented and screw-retained implant reconstructions: a systematic review of the survival and complication rates. → Clin Oral Implants Res. 2012 Oct;23 Suppl 6:163–201.
Recently, the conometric connection was proposed as a fixation system for IFDPs. Such a system is composed of a tapered coping fixed to the prosthesis and inserted into a tapered abutment. When a suitable insertion force is applied, this system is capable of providing a fixed connection.7Bressan E, Lops D, Tomasi C, Ricci S, Stocchero M, Carniel EL. Experimental and computational investigation of Morse taper conometric system reliability for the definition of fixed connections between dental implants and prostheses. → Proc Inst Mech Eng H. 2014 Jul;228(7):674–81. Such retention is based on the friction between the components, without the use of cement. The clinical use of the conometric retention has been described for implant-supported complete8Bressan E, Lops D. Conometric retention for complete fixed prosthesis supported by four implants: 2-years prospective study. → Clin Oral Implants Res. 2014 May;25(5):546–52. and partial9Degidi M, Nardi D, Piattelli A. The conometric concept: coupling connection for immediately loaded titanium-reinforced provisional fixed partial dentures—a case series. → Int J Periodontics Restorative Dent. 2016 May–Jun;36(3):347–54. fixed prostheses.
One of the reported advantages of a conometric connection system is the retrievability of the restoration.10Bressan E, Lops D. Conometric retention for complete fixed prosthesis supported by four implants: 2-years prospective study. → Clin Oral Implants Res. 2014 May;25(5):546–52. Conometric-retained prostheses can be easily removed by the operator in order to check the periimplant soft-tissue status and for periodic hygiene procedures. Despite the promising results in terms of clinical success, long-term studies on mandibular full-arch conometric-retained restorations with a larger study population are lacking in the current literature. Thus, the aim of the present retrospective study was to assess the clinical performance of implant-supported mandibular complete fixed prostheses with conometric retention after 3 years of functional loading. Outcomes were evaluated in terms of implant and prosthetic survival, marginal bone loss and incidence of technical complications.
Materials and methods
In this retrospective study, patients consecutively treated with implant-supported mandibular complete fixed prostheses with conometric retention were selected. The IFDPs were supported by 4 mandibular implants placed in each patient. All cases were treated in a single center and had 3 years of follow-up from the time of prosthesis delivery. This study was conducted according to the principles of the Declaration of Helsinki on human medical experimentation. All patients signed informed consent prior to the implant treatment.
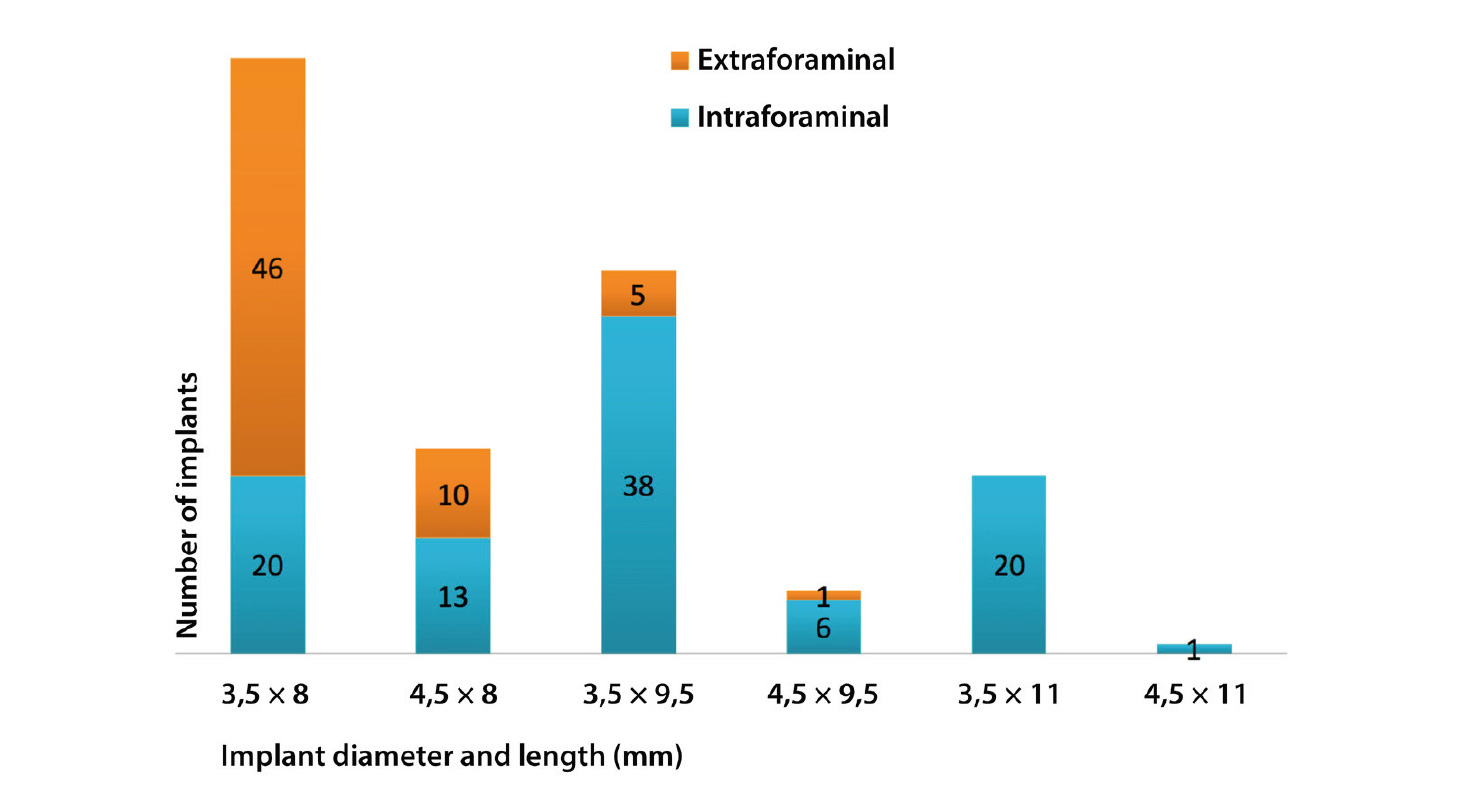
The adopted surgical and prosthetic protocol has been described in a previous study.11Bressan E, Lops D. Conometric retention for complete fixed prosthesis supported by four implants: 2-years prospective study. → Clin Oral Implants Res. 2014 May;25(5):546–52. After prosthetic delivery (baseline, T0), patients were recalled at 6 months, 1 year, 2 years and 3 years (T3) for follow-up visits. At each visit, the prosthesis was removed and oral hygiene, implant maintenance and patient-centered motivational instruction were delivered. Data were extracted from patient files at T3. Variables were subdivided between patient-based and implant-based. The following patient demographic characteristics were reported: sex, age at the time of surgery, smoking habit, bruxism, drug intake, systemic disease and time of prosthetic loading. Implant information, such as diameter and length, were recorded. Moreover, intraforaminal (positions .1, .2, .3, .4) or extraforaminal (positions .5, .6, .7) implant position was recorded (Fig. 1). Implant failure and technical complications, such as loss of retention, veneer fracture, need for relining and framework fracture, that occurred during the period of function were recorded. Standardized radiographic examinations with the use of a Rinn Universal Collimator (Dentsply Sirona, York, Pa., U.S.) were performed to assess the marginal bone. Radiographs were acquired at T0 and at T3. For marginal bone assessments, ImageJ software (Version 1.48, National Institutes of Health, Bethesda, Md., U.S.) was used. The measurements were performed with a precision of 0.01 mm at a 7× digital magnification level. For each analyzed radiograph, measurement calibration was carried out using the diameter and length of the implant. Then, the distance from the implant shoulder to the first appreciable contact point between the bone and implant was measured. In cases where the marginal bone level was coronal or at the level of the implant shoulder, the reported value was 0 mm. The measurement was performed both medial and distal to the implant. The mean mesial and distal values were calculated at T0 and T3. The radiographic analysis was performed in a blind manner by 1 experienced examiner not involved in the study. Marginal bone loss (MBL) was calculated as the difference between the 2 time points.
Number of implants based on diameter and length. The intra-arch position is distinguished.
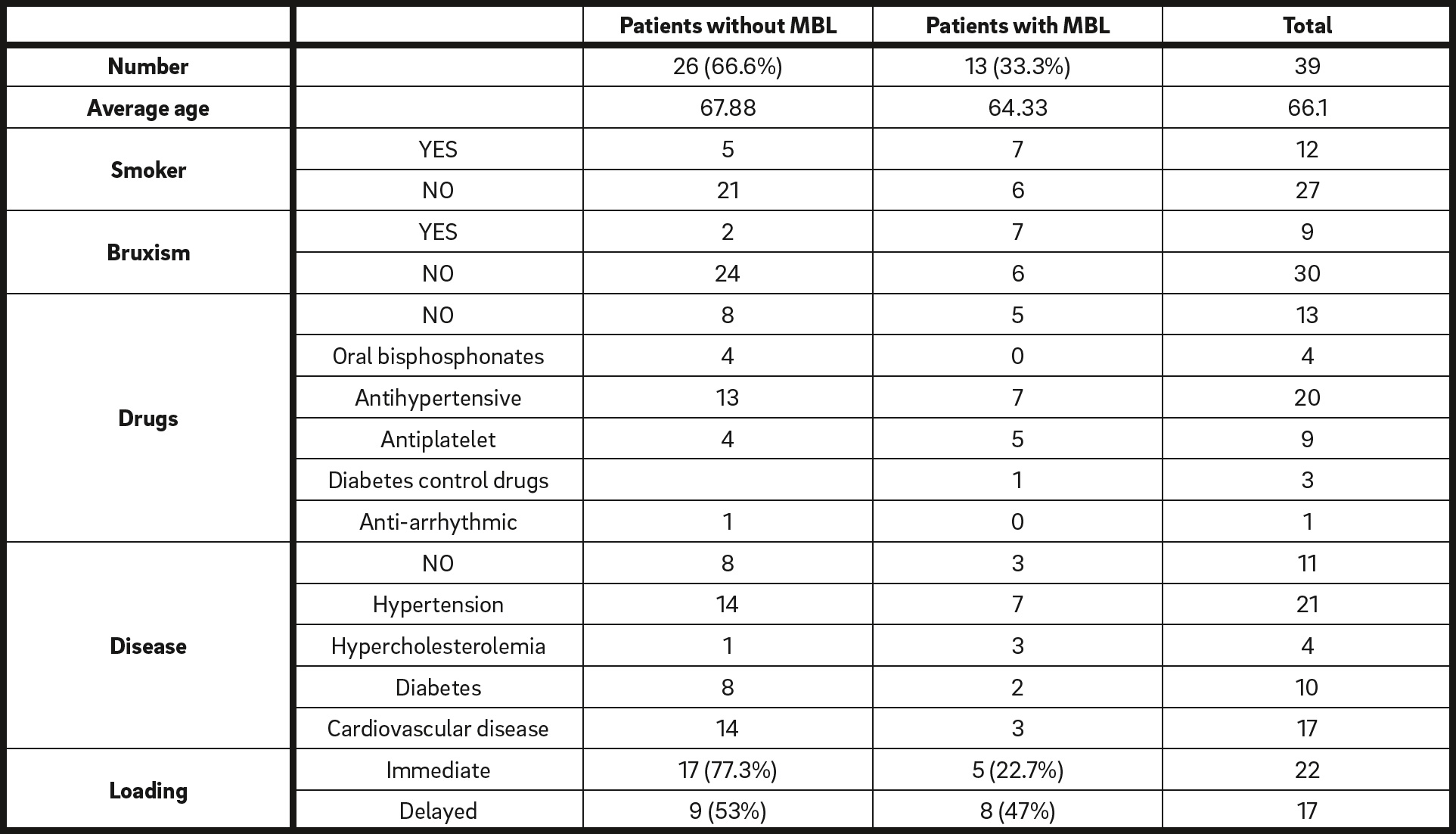
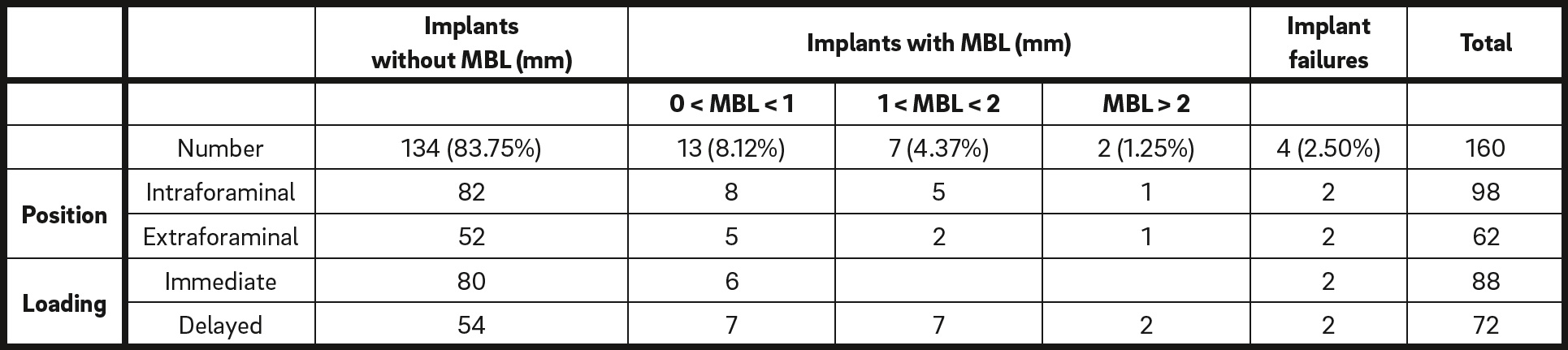
According to the MBL results, patient-based variables were subdivided in 2 categories: patients with no MBL and patients who presented with MBL (Table 1). In the same manner, implant-based variables were subdivided into the following categories: implants with no MBL, implants with an MBL of < 1 mm, implants with an MBL of between 1 and 2 mm, implants with an MBL of > 2 mm, and implant failure (Table 2). Moreover, the incidence of technical complications was calculated.
Results
Thirty-nine patients (19 men and 20 women) were enrolled in the study. Demographic characteristics are shown in Table 1. A total of 160 implants were placed, 98 intraforaminally and 62 extraforaminally (Fig. 1). There was no sign of MBL around 83.75% of the implants, while 2.5% were lost during the 3-year follow-up. Implantbased variables according to MBL can be found in Table 2. Mucositis in 1 patient was encountered during periodic follow-up (Fig. 2). Regarding the restorations, 71.8% were free of technical complications during the entire follow-up period. Complications that occurred in restorations were veneer fracture, framework fracture, loss of retention and need for relining (Table 3; Fig. 3).
Discussion
In the present retrospective study, 39 patients with complete mandibular edentulism were rehabilitated with implant-supported conometric-retained prostheses. Our aim was to report the clinical performance in terms of incidence of technical and biological complications in a 3-year follow-up period. For this purpose, we included data on both immediate and delayed loading. The rehabilitation of edentate mandibles with implant-supported fixed restoration has been reported in long-term studies since the 1990s.12Lindquist LW, Carlsson GE, Jemt T. A prospective 15-year follow-up study of mandibular fixed prostheses supported by osseointegrated implants. Clinical results and marginal bone loss. → Clin Oral Implants Res. 1996 Dec;7(4):329–36. Despite the high success rates after 15 years, several surgical and prosthetic procedures have been introduced over the years in terms of number of supporting implants, intra-arch locations, time of loading, and type of connection between the implant and the prosthesis.13Weber HP, Morton D, Gallucci GO, Roccuzzo M, Cordaro L, Grutter L. Consensus statements and recommended clinical procedures regarding loading protocols. → Int J Oral Maxillofac Implants. 2009;24 Suppl:180–3.
A meta-analysis on mandibular IFDPs14Papaspyridakos P, Mokti M, Chen CJ, Benic GI, Gallucci GO, Chronopoulos V. Implant and prosthodontic survival rates with implant fixed complete dental prostheses in the edentulous mandible after at least 5 years: a systematic review. → Clin Implant Dent Relat Res. 2014 Oct;16(5):705–17. investigated the implant survival rate of restorations supported by a range of 4–9 implants. In that study, 17 trials, including 501 patients and 2,827 implants, were considered. According to the results, intraforaminal implant placement was the most common technique (88.5% of all implants). In the present study, all restorations were supported by 4 implants, which were placed either intraforaminally or extraforaminally. Implants in the distal position were placed posterior to the mental foramen whenever the bone amount was sufficient in order to reduce the distal cantilever.
Patient demographic characteristics and patientbased variables. Data are shown as frequency (percentage of the total).
Implant-based variables according to marginal bone loss (MBL) and implant failure.
Occurrence of technical complications in the restorations. Data are shown as frequency (percentage of the total).
The majority of implants were placed in the intraforaminal area; however, 62 implants were placed distal to the foramen. A total of 33 restorations were supported by at least 2 extraforaminal implants. This means that in the majority of cases (65%) the placement of implants of at least 8 mm in length was possible in the distal sites. This is in accordance with a recent study that evaluated the dimensions of the alveolar ridge in the edentulous posterior mandible15Bressan E, Ferrarese N, Pramstraller M, Lops D, Farina R, Tomasi C. Ridge dimensions of the edentulous mandible in posterior sextants: an observational study on cone beam computed tomography radiographs. → Implant Dent. 2017 Feb;26(1):66–72. based on CBCT data. A mean bone height of 11.20 mm and 10.28 mm in the sites of the second premolar and mesial root of the first molar, respectively, was measured.
During the present 3-year follow-up study, 4 out of 160 implants failed. Therefore, the overall implant survival rate was 97.5%. In all cases, implants were lost during the first year after placement. This result is in accordance with recent studies with similar groups of patients and follow-up.16Sanz M, Ivanoff CJ, Weingart D, Wiltfang J, Gahlert M, Cordaro L, Ganeles J, Bragger U, Jackowski J, Martin WC, Jung RE, Chen S, Hammerle C. Clinical and radiologic outcomes after submerged and transmucosal implant placement with two-piece implants in the anterior maxilla and mandible: 3-year results of a randomized controlled clinical trial. → Clin Implant Dent Relat Res. 2015 Apr;17(2):234–46.17Agliardi EL, Pozzi A, Stappert CF, Benzi R, Romeo D, Gherlone E. Immediate fixed rehabilitation of the edentulous maxilla: a prospective clinical and radiological study after 3 years of loading. → Clin Implant Dent Relat Res. 2014 Apr;16(2):292–302. In addition, a systematic review showed similar results.18Papaspyridakos P, Mokti M, Chen CJ, Benic GI, Gallucci GO, Chronopoulos V. Implant and prosthodontic survival rates with implant fixed complete dental prostheses in the edentulous mandible after at least 5 years: a systematic review. → Clin Implant Dent Relat Res. 2014 Oct;16(5):705–17. In the study, the cumulative implant survival rate estimates were calculated based on the number of supporting implants for mandibular full-arch restorations. At the 5-year endpoint for restorations supported on 4 implants, the implant survival rate was 97.65% (95% CI: 94.48–100). Regarding biological complications, a good performance in terms of incidence of MBL was observed in the present study, since 134 out of the 156 surviving implants (85.9%) did not show any MBL after the 3-year follow-up. However, as previous studies observed, the stability of marginal bone is related to patient-related factors.19Herrmann I, Lekholm U, Holm S, Kultje C. Evaluation of patient and implant characteristics as potential prognostic factors for oral implant failures. → Int J Oral Maxillofac Implants. 2005 Mar–Apr;20(2):220–30.
One patient presented with periimplant mucositis affecting 2 implants (in positions #32 and 35). This biological complication was successfully treated with interceptive supportive therapy.
From our results, a relevant difference in the incidence of MBL was observed based on smoking habit, since it occurred in 58.30% of the smoking patients, while it occurred only in 28.57% of the nonsmoking patients. It is well known that placing implants in smoking patients has always been a challenging situation, as many clinical studies have shown a lower implant success rate in this regard. In a systematic review on the effect of smoking habit,20Chrcanovic BR, Albrektsson T, Wennerberg A. Smoking and dental implants: a systematic review and meta-analysis. → J Dent. 2015 May;43(5):487–98. 15 observational studies with a follow-up period ranging from 8 to 240 months were included. A total of 5,840 implants placed in smoking patients were compared with 14, 683 placed in nonsmoking patients. The authors concluded that the risk of MBL is higher in smokers, especially in the maxillary bone.21Chrcanovic BR, Albrektsson T, Wennerberg A. Smoking and dental implants: a systematic review and meta-analysis. → J Dent. 2015 May;43(5):487–98.
In the present study, at periodic follow-up visits, the prostheses were removed in order to check the periimplant soft-tissue status. Mucositis affecting two implants was successfully treated with interceptive supportive therapy. The protocol adopted consisted of professional oral hygiene followed by the use of a 0.2% chlorhexidine mouthrinse 3 times per day for 2 weeks. Therefore, the easy retrievability of the restoration facilitated primary and secondary prevention of periimplant diseases.

Fig. 3
The most severe technical complication encountered in this study was framework fracture. Two cases in which a crack occurred in the distal cantilever are shown.
It is well known that occurrence of complications for full-arch restoration is relevant.22Sailer I, Mühlemann S, Zwahlen M, Hämmerle CH, Schneider D. Cemented and screw-retained implant reconstructions: a systematic review of the survival and complication rates. → Clin Oral Implants Res. 2012 Oct;23 Suppl 6:163–201.23Aglietta M, Siciliano VI, Zwahlen M, Bragger U, Pjetursson BE, Lang NP, Salvi GE. A systematic review of the survival and complication rates of implant supported fixed dental prostheses with cantilever extensions after an observation period of at least 5 years. → Clin Oral Implants Res. 2009 May;20(5):441–51. In a systematic review by Papaspyridakos et al., the cumulative rate of prostheses free of complications was 29.3% at the 5-year follow-up.24Papaspyridakos P, Mokti M, Chen CJ, Benic GI, Gallucci GO, Chronopoulos V. Implant and prosthodontic survival rates with implant fixed complete dental prostheses in the edentulous mandible after at least 5 years: a systematic review. → Clin Implant Dent Relat Res. 2014 Oct;16(5):705–17. Interestingly, the estimated cumulative rates of screw fracture and screw loosening complications were 10.4% and 9.3%, respectively. In contrast, in the present study, the percentage of restorations free of technical complications was 71.8% at 3 years. A reason for this result could be the prosthetic design adopted: The avoidance of screws might have had a major role in decreasing the incidence of technical complications.
The most severe technical complication encountered in this study was framework fracture. Cracks were located in the distal cantilever in all 3 cases. This result is not surprising, since it is generally accepted that the incidence rate of prosthetic complications is increased dramatically when distal extensions are applied.25Brägger U, Hirt-Steiner S, Schnell N, Schmidlin K, Salvi GE, Pjetursson B, Matuliene G, Zwahlen M, Lang NP. Complication and failure rates of fixed dental prostheses in patients treated for periodontal disease. → Clin Oral Implants Res. 2011 Jan;22(1):70–7. In cases of framework fracture, the prosthesis was removed and then repaired. In order to reduce this occurrence, a distal cantilever is to be avoided whenever anatomical structures allow it. Thus, the positioning of distal implants posterior to the mental foramen is advocated. Interestingly, all patients in which framework fractures occurred were bruxers. These results are in accordance with previous studies found in the literature in which many prosthodontic failures were associated with bruxism.26Mikeli A, Walter MH. Impact of bruxism on ceramic defects in implant-borne fixed dental prostheses: a retrospective study. → Int J Prosthodont. 2016 May–Jun;29(3):296–8.27Chrcanovic BR, Kisch J, Albrektsson T, Wennerberg A. Bruxism and dental implant failures: a multilevel mixed effects parametric survival analysis approach. → J Oral Rehabil. 2016 Nov;43(11):813–23. Other minor technical complications were veneer fracture (n = 4), loss of retention (n = 2) and need for relining (n = 2). In all cases, the problem was addressed after easy removal. Direct veneer repair, coping replacement and indirect relining were provided respectively.
One major limitation of the study was that immediate and delayed loading restorations were included in the same study. However, since the aim of this study was to record the performance of a specific prosthetic protocol, it is believed that different clinical procedures could give a wider picture. Moreover, the substantially similar behavior of immediate and delayed loading implants justifies a direct comparison.
With the present retrospective study, a good clinical performance after 3 years of follow-up in terms of survival rate, marginal bone resorption, and incidence of biological and technical complications was observed. One of the major advantages was the effortless retrievability of the restoration, which facilitated primary and secondary prevention. As a matter of fact, with the periodic prosthesis removal for routine hygiene procedures, periimplant disease at early stages could be intercepted and technical complications could be easily solved.
Conclusion
Within the limitations of the study, the clinical performance of implant-supported mandibular complete fixed prostheses with conometric retention after 3 years of functional loading showed a low rate of MBL and technical complications. Owing to the easy retrievability of the system, all complications were successfully addressed. A careful patient selection must be undertaken, since bruxism and distal cantilever may represent risk factors for major technical complications such as framework fracture. The efficacy of this treatment option in terms of cost and maintenance has to be confirmed by multicenter, longer-term studies.
Competing interests
The authors declare that they have no competing interests.
Why did you conduct the research reported on in this paper?
For what reasons could others cite your paper?
How could your study’s findings have an impact on dentistry?
What is the relevance of your study’s findings to the daily practice of a dentist?
What are your recommendations for further investigation of the topic of your article?
References
| 1. | ↑ | Pjetursson BE, Asgeirsson AG, Zwahlen M, Sailer I. Improvements in implant dentistry over the last decade: comparison of survival and complication rates in older and newer publications. → Int J Oral Maxillofac Implants. 2014;29 Suppl:308–24. |
| 2, 6, 22. | ↑ | Sailer I, Mühlemann S, Zwahlen M, Hämmerle CH, Schneider D. Cemented and screw-retained implant reconstructions: a systematic review of the survival and complication rates. → Clin Oral Implants Res. 2012 Oct;23 Suppl 6:163–201. |
| 3. | ↑ | Pjetursson BE, Thoma D, Jung R, Zwahlen M, Zembic A. A systematic review of the survival and complication rates of implant-supported fixed dental prostheses (FDPs) after a mean observation period of at least 5 years. → Clin Oral Implants Res. 2012 Oct;23 Suppl 6:22–38. |
| 4. | ↑ | Proussaefs P, AlHelal A. The combination prosthesis: a digitally designed retrievable cement- and screw-retained implant-supported prosthesis. → J Prosthet Dent. 2018 Apr;119(4):535–9. Epub 2017 Sep 18. |
| 5. | ↑ | Shadid R, Sadaqa N. A comparison between screw- and cement-retained implant prostheses. A literature review. → J Oral Implantol. 2012 Jun;38(3):298–307. |
| 7. | ↑ | Bressan E, Lops D, Tomasi C, Ricci S, Stocchero M, Carniel EL. Experimental and computational investigation of Morse taper conometric system reliability for the definition of fixed connections between dental implants and prostheses. → Proc Inst Mech Eng H. 2014 Jul;228(7):674–81. |
| 8, 10, 11. | ↑ | Bressan E, Lops D. Conometric retention for complete fixed prosthesis supported by four implants: 2-years prospective study. → Clin Oral Implants Res. 2014 May;25(5):546–52. |
| 9. | ↑ | Degidi M, Nardi D, Piattelli A. The conometric concept: coupling connection for immediately loaded titanium-reinforced provisional fixed partial dentures—a case series. → Int J Periodontics Restorative Dent. 2016 May–Jun;36(3):347–54. |
| 12. | ↑ | Lindquist LW, Carlsson GE, Jemt T. A prospective 15-year follow-up study of mandibular fixed prostheses supported by osseointegrated implants. Clinical results and marginal bone loss. → Clin Oral Implants Res. 1996 Dec;7(4):329–36. |
| 13. | ↑ | Weber HP, Morton D, Gallucci GO, Roccuzzo M, Cordaro L, Grutter L. Consensus statements and recommended clinical procedures regarding loading protocols. → Int J Oral Maxillofac Implants. 2009;24 Suppl:180–3. |
| 14, 18, 24. | ↑ | Papaspyridakos P, Mokti M, Chen CJ, Benic GI, Gallucci GO, Chronopoulos V. Implant and prosthodontic survival rates with implant fixed complete dental prostheses in the edentulous mandible after at least 5 years: a systematic review. → Clin Implant Dent Relat Res. 2014 Oct;16(5):705–17. |
| 15. | ↑ | Bressan E, Ferrarese N, Pramstraller M, Lops D, Farina R, Tomasi C. Ridge dimensions of the edentulous mandible in posterior sextants: an observational study on cone beam computed tomography radiographs. → Implant Dent. 2017 Feb;26(1):66–72. |
| 16. | ↑ | Sanz M, Ivanoff CJ, Weingart D, Wiltfang J, Gahlert M, Cordaro L, Ganeles J, Bragger U, Jackowski J, Martin WC, Jung RE, Chen S, Hammerle C. Clinical and radiologic outcomes after submerged and transmucosal implant placement with two-piece implants in the anterior maxilla and mandible: 3-year results of a randomized controlled clinical trial. → Clin Implant Dent Relat Res. 2015 Apr;17(2):234–46. |
| 17. | ↑ | Agliardi EL, Pozzi A, Stappert CF, Benzi R, Romeo D, Gherlone E. Immediate fixed rehabilitation of the edentulous maxilla: a prospective clinical and radiological study after 3 years of loading. → Clin Implant Dent Relat Res. 2014 Apr;16(2):292–302. |
| 19. | ↑ | Herrmann I, Lekholm U, Holm S, Kultje C. Evaluation of patient and implant characteristics as potential prognostic factors for oral implant failures. → Int J Oral Maxillofac Implants. 2005 Mar–Apr;20(2):220–30. |
| 20, 21. | ↑ | Chrcanovic BR, Albrektsson T, Wennerberg A. Smoking and dental implants: a systematic review and meta-analysis. → J Dent. 2015 May;43(5):487–98. |
| 23. | ↑ | Aglietta M, Siciliano VI, Zwahlen M, Bragger U, Pjetursson BE, Lang NP, Salvi GE. A systematic review of the survival and complication rates of implant supported fixed dental prostheses with cantilever extensions after an observation period of at least 5 years. → Clin Oral Implants Res. 2009 May;20(5):441–51. |
| 25. | ↑ | Brägger U, Hirt-Steiner S, Schnell N, Schmidlin K, Salvi GE, Pjetursson B, Matuliene G, Zwahlen M, Lang NP. Complication and failure rates of fixed dental prostheses in patients treated for periodontal disease. → Clin Oral Implants Res. 2011 Jan;22(1):70–7. |
| 26. | ↑ | Mikeli A, Walter MH. Impact of bruxism on ceramic defects in implant-borne fixed dental prostheses: a retrospective study. → Int J Prosthodont. 2016 May–Jun;29(3):296–8. |
| 27. | ↑ | Chrcanovic BR, Kisch J, Albrektsson T, Wennerberg A. Bruxism and dental implant failures: a multilevel mixed effects parametric survival analysis approach. → J Oral Rehabil. 2016 Nov;43(11):813–23. |




Leave a Reply
Be the First to Comment!